aripiprazol-atipichn-y-antipsihotik-s-nov-m-mehanizmom-deystviya-i-risperidon-v-sravnenii-s-platsebo-u-boln-h-shizofreniey-i-shizoaffektivn-m-rasstroystvom (2)
реклама

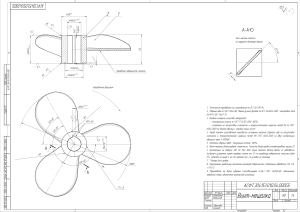
ÓÄÊ 616.895.8–085:615.214 ÀÐÈÏÈÏÐÀÇÎË, ÀÒÈÏÈ×ÍÛÉ ÀÍÒÈÏÑÈÕÎÒÈÊ Ñ ÍÎÂÛÌ ÌÅÕÀÍÈÇÌÎÌ ÄÅÉÑÒÂÈß, È ÐÈÑÏÅÐÈÄÎÍ Â ÑÐÀÂÍÅÍÈÈ Ñ ÏËÀÖÅÁÎ Ó ÁÎËÜÍÛÕ ØÈÇÎÔÐÅÍÈÅÉ È ØÈÇÎÀÔÔÅÊÒÈÂÍÛÌ ÐÀÑÑÒÐÎÉÑÒÂÎÌ* Ñ. Ã. Ïîòêèí, A. Ð. Ñàõà, M. Äæ. Êóÿâà, Ó. Õ. Êàðñîí, M. Àëè, Ý. Ñòîê, Äæ. Ñòðèíãôåëëîó, Ã. Èíãåíèòî, Ñ. Ð. Ìàðäåð Ìåõàíèçìû äåéñòâèÿ àòèïè÷íûõ àíòèïñèõîòèêîâ øèðîêî îñâåùåíû â ëèòåðàòóðå (11, 16, 17, 19, 24– 27, 31–33, 35). Ðàçðàáîòêà ÷àñòè÷íûõ àãîíèñòîâ D2-ðåöåïòîðîâ ÿâëÿåòñÿ ëîãè÷åñêèì ïðîäîëæåíèåì íîâûõ ïîäõîäîâ ê ôàðìàêîòåðàïèè øèçîôðåíèè, òàê êàê ñ÷èòàåòñÿ, ÷òî ïàòîôèçèîëîãè÷åñêèå ìåõàíèçìû ðàçâèòèÿ øèçîôðåíèè îñíîâàíû íà èçáûòî÷íîé äîôàìèíîâîé àêòèâíîñòè â îäíèõ îáëàñòÿõ ãîëîâíîãî ìîçãà è íåäîñòàòî÷íîé àêòèâíîñòè â äðóãèõ îáëàñòÿõ. ×àñòè÷íûå àãîíèñòû D2-ðåöåïòîðîâ ìîãóò âûñòóïàòü â êà÷åñòâå ôóíêöèîíàëüíûõ àíòàãîíèñòîâ â îáëàñòÿõ ñ âûñîêèì ñîäåðæàíèåì äîôàìèíà, íàïðèìåð, â ìåçîëèìáè÷åñêîì ïóòè, íå ÿâëÿÿñü òàêîâûìè â îáëàñòÿõ ñ íîðìàëüíûì óðîâíåì äîôàìèíà (íèãðîñòðèàðíûé è òóáåðîèíôóíäèáóëÿðíûé ïóòè). Òàêèì îáðàçîì, îæèäàåòñÿ, ÷òî ÷àñòè÷íûå àãîíèñòû D2-ðåöåïòîðîâ áóäóò âîçäåéñòâîâàòü íà ïðîäóêòèâíóþ ñèìïòîìàòèêó, íå âûçûâàÿ äâèãàòåëüíûå ðàññòðîéñòâà è ãèïåðïðîëàêòèíåìèþ.  îáëàñòÿõ ñî ñíèæåííîé êîíöåíòðàöèåé äîôàìèíà, íàïðèìåð, â ìåçîêîðòèêàëüíîì ïóòè, ÷àñòè÷íûé àãîíèñò D2-ðåöåïòîðîâ ïðîÿâèò ôóíêöèîíàëüíóþ àãîíèñòè÷åñêóþ àêòèâíîñòü. Ïîêàçàíî, ÷òî àðèïèïðàçîë â óñëîâèÿõ in vitro îáíàðóæèâàåò ÷àñòè÷íóþ àãîíèñòè÷åñêóþ àêòèâíîñòü â îòíîøåíèè êëîíèðîâàííûõ D2-ðåöåïòîðîâ ÷åëîâåêà (8).  îòñóòñòâèè äîôàìèíà, ïðåïàðàò àêòèâèðóåò D2-ðåöåïòîðû, ÷òî óâåëè÷èâàåò ðåöåïòîðíóþ àêòèâíîñòü; ñòåïåíü âûðàæåííîñòè ýòîé àêòèâíîñòè, îäíàêî, íåñêîëüêî ìåíüøå, ÷åì ó äîôàìèíà. Åñëè äîôàìèí ïðèñóòñòâóåò, àðèïèïðàçîë èíãèáèðóåò åãî ñâÿçûâàíèå ñ D2-ðåöåïòîðàìè, ÷òî ñíèæàåò ðåöåïòîðíóþ àêòèâíîñòü; â ñâÿçè ñ îñîáûì ìåõàíèçìîì äåéñòâèÿ, ïðèñóùèì àðèïèïðàçîëó, àêòèâàöèÿ D2-ðåöåïòîðîâ íå áëîêèðóåòñÿ ïîëíîñòüþ (8).  ýêñïåðèìåíòàõ ex vivo, àðèïèïðàçîë èíãèáèðîâàë ñïîíòàííûé âûáðîñ ïðîëàêòèíà â ãèïîôèçå (13). Ýòî èíãèáèðîâàíèå áûëî çíà÷èòåëüíî ìåíüøèì â ñðàâíåíèè ñ òåì, ÷òî äîñòèãàëîñü ïîëíûì àãîíèñòîì äîôàìèíîâûõ D2-ðåöåïòîðîâ – òàëèïåêñîëîì, è ìîãëî áûòü ïîëíîñòüþ áëîêèðîâàíî ãàëîïåðèäîëîì.  óñëîâèÿõ in vivo àðèïèïðàçîë äåìîíñòðèðóåò ýôôåêò àíòàãîíèñòà D2-ðåöåïòîðîâ íà ìîäåëÿõ æèâîòíûõ ñ äîôàìèíåðãè÷åñêîé ãèïåðàêòèâíîñòüþ (íàïðèìåð, áëîêàäà ñòåðåîòèïèè, âûçâàííîé àïîìîðôèí ãèäðîõëîðèäîì) è àãîíèñòà D2-ðåöåïòîðîâ íà ìîäåëÿõ ñ äîôàìèíåðãè÷åñêîé ãèïîàêòèâíîñòüþ (èíãèáèðîâàíèå ïîâûøåííîãî ñèíòåçà ïðîëàêòèíà ó êðûñ, ëå÷åííûõ ðåçåðïèíîì) (18). Àðèïèïðàçîë îáíàðóæèâàåò ÷àñòè÷íóþ àãîíèñòè÷åñêóþ àêòèâíîñòü â îòíîøåíèè 5HT1A-ðåöåïòîðîâ (14). Ïðåäïîëàãàåòñÿ, ÷òî ÷àñòè÷íàÿ àãîíèñòè÷åñêàÿ àêòèâíîñòü â îòíîøåíèè 5HT1A-ðåöåïòîðîâ â öåëîì îáóñëîâëèâàåò ïîëîæèòåëüíîå âîçäåéñòâèå íà ñèìïòîìàòèêó, íàáëþäàåìóþ ó áîëüíûõ øèçîôðåíèè, âêëþ÷àÿ òðåâîãó, äåïðåññèþ, êîãíèòèâíûå è íåãàòèâíûå ðàññòðîéñòâà (14). Òàêæå áûëî ïîêàçàíî, ÷òî àðèïèïðàçîë îáëàäàåò àíòàãîíèñòè÷åñêîé àêòèâíîñòüþ â îòíîøåíèè 5HT2A-ðåöåïòîðîâ (23), ñðàâíèìîé ñ òàêîâîé ó äðóãèõ àòèïè÷íûõ àíòèïñèõîòèêîâ. Ïðåäïîëàãàåòñÿ, ÷òî àíòàãîíèñòè÷åñêàÿ àêòèâíîñòü â îòíîøåíèè 5HT2A-ðåöåïòîðîâ îáóñëîâëèâàåò íèçêóþ ÷àñòîòó ðàçâèòèÿ ÝÏÑ (1) è ïîëîæèòåëüíîå âëèÿíèå íà íåãàòèâíûå ðàññòðîéñòâà (21, 30). Öåëüþ íàñòîÿùåãî èññëåäîâàíèÿ ÿâëÿëîñü èçó÷åíèå ýôôåêòèâíîñòè, áåçîïàñíîñòè è ïåðåíîñèìîñòè àðèïèïðàçîëà â äîçèðîâêå 20 ìã è 30 ìã ïðè ëå÷åíèè îñòðûõ ïñèõîòè÷åñêèõ ñîñòîÿíèé ó áîëüíûõ øèçîôðåíèåé èëè øèçîàôôåêòèâíûì ðàññòðîéñòâîì, ñ îöåíêîé âëèÿíèÿ ïðåïàðàòà íà íåãàòèâíûå ðàññòðîéñòâà è îïðåäåëåíèÿ âçàèìîñâÿçè ìåæäó äîçèðîâêîé ïðåïàðàòà è ðàçâèòèåì ïîëîæèòåëüíîãî îòâåòà. Ðèñïåðèäîí èñïîëüçîâàëñÿ â êà÷åñòâå àêòèâíîãî êîíòðîëÿ äëÿ îöåíêè îòâåòà íà òåðàïèþ. Äèçàéí èññëåäîâàíèÿ íå ïðåäïîëàãàë îöåíêó ðàçëè÷èé â ýôôåêòèâíîñòè òåðàïèè â ðàçíûõ òåðàïåâòè÷åñêèõ ãðóïïàõ. * Ðàñøèðåííûé ðåôåðàò ñòàòüè, îïóáëèêîâàííîé â Arch. Gen. Psychiatry. – 2003. – Vol. 60. – P. 681–690. 72 (òÿæåñòü), êðàòêîé øêàëå ïñèõèàòðè÷åñêîé îöåíêè (BPRS) è ñðåäíåå çíà÷åíèå øêàëû CGI-I (óëó÷øåíèå). Òàêæå ó÷èòûâàëîñü êîëè÷åñòâî ðåñïîíäåðîâ (ïàöèåíòû ñî ñíèæåíèåì îáùåãî áàëëà ïî øêàëå PANSS íà ≥30% èëè áîëüíûå, ÷ü¸ ñîñòîÿíèå ñîîòâåòñòâîâàëî ïóíêòó 1 èëè 2 ïî øêàëå CGI-I). Îöåíêà áåçîïàñíîñòè. Ïàðêèíñîíèçì, àêàòèçèÿ è äèñêèíåçèÿ îöåíèâàëèñü ñ ïîìîùüþ ñòàíäàðòèçîâàííûõ øêàë äëÿ îöåíêè ÝÏÑ: øêàëû ÑèìïñîíàÀíãóñà (SAS), øêàëû îöåíêè àêàòèçèè Áàðíñà (BAS) è øêàëû ïàòîëîãè÷åñêèõ íåïðîèçâîëüíûõ äâèæåíèé (AIMS) ñîîòâåòñòâåííî. Âèòàëüíûå ïîêàçàòåëè (ïóëüñ, ñèñòîëè÷åñêîå è äèàñòîëè÷åñêîå àðòåðèàëüíîå äàâëåíèå) îöåíèâàëèñü íà ýòàïå ñêðèíèíãà, â íà÷àëå èññëåäîâàíèÿ, â 1–5, 14 è 28 äíè. Âåñ òåëà è óðîâåíü ïðîëàêòèíà â ïëàçìå êðîâè îöåíèâàëèñü â íà÷àëå èññëåäîâàíèÿ, íà 14 è 28 äíè. Ýëåêòðîêàðäèîãðàôè÷åñêîå îáñëåäîâàíèå è îöåíêà ëàáîðàòîðíûõ ïîêàçàòåëåé ïðîâîäèëèñü íà ýòàïå ñêðèíèíãà, â íà÷àëå èññëåäîâàíèÿ (êðîìå ÝÊÃ), íà 14 è 28 äíè. Ñîïóòñòâóþùàÿ ëåêàðñòâåííàÿ òåðàïèÿ. Íå ðàçðåøàëîñü íàçíà÷åíèå èíûõ ïñèõîòðîïíûõ ïðåïàðàòîâ, êðîìå èññëåäóåìûõ, çà èñêëþ÷åíèåì ëîðàçåïàìà (äëÿ êóïèðîâàíèÿ òðåâîãè èëè èíñîìíèè), â òîì ÷èñëå âíóòðèìûøå÷íîé ôîðìû ïðè îñòðîé àæèòàöèè. Èñïîëüçîâàíèå áåíçòðîïèíà äëÿ êîððåêöèè ýêñòðàïèðàìèäíûõ ðàññòðîéñòâ äîïóñêàëîñü â äîçå, íå ïðåâûøàþùåé 6 ìã/ñóò. Ñòàòèñòè÷åñêèå ïðîöåäóðû. Ïåðâè÷íûé àíàëèç ýôôåêòèâíîñòè áûë îñíîâàí íà äàííûõ ïîëó÷åííûõ âî âðåìÿ ïîñëåäíåãî âèçèòà ïàöèåíòà, íåçàâèñèìî îò òîãî çàâåðøèë îí èññëåäîâàíèå èëè íåò (ïðè àíàëèçå ó÷èòûâàëè ïîñëåäíþþ îöåíêó ñîñòîÿíèÿ, åñëè îíà ïðîâîäèëàñü äî ïëàíîâîãî çàâåðøåíèÿ èññëåäîâàíèÿ – ìåòîä LOCF). Ïåðâè÷íîå ñðàâíåíèå òåðàïèè âêëþ÷àëî ñîïîñòàâëåíèå òåðàïèè 20 ìã àðèïèðàçîëà vs ïëàöåáî è 30 ìã àðèïèïðàçîëà vs ïëàöåáî. Äàííûå àíàëîãîâîé ýôôåêòèâíîñòè (èçìåíåíèÿ ïîêàçàòåëåé ñ èñõîäíûõ çíà÷åíèé) áûëè îöåíåíû ñ èñïîëüçîâàíèåì êîâàðèàöèîííîãî àíàëèçà, ñ âêëþ÷åíèåì èñõîäíûõ çíà÷åíèé è öåíòðà â êà÷åñòâå ôàêòîðîâ. Äàííûå êàòåãîðèàëüíîé ýôôåêòèâíîñòè (êîëè÷åñòâî áàëëîâ ïî CGI-I è ðåñïîíäåðû) àíàëèçèðîâàëè òåñòîì Cochran-Mantel-Haenzel. Îöåíêó ýôôåêòèâíîñòè ìåæäó ñðàâíèâàåìûìè ãðóïïàìè ïðîâîäèëè ïî íèñõîäÿùåé ïðîöåäóðå, òàê, íàïðèìåð, ñðàâíèâàëè 30 ìã àðèïèïðàçîëà ñ ïëàöåáî äâóñòîðîííèìè òåñòàìè ñ óðîâíåì äîñòîâåðíîñòè 0,05; â ñëó÷àå îòêëîíåíèÿ, ñðàâíèâàëè 20 ìã àðèïèïðàçîëà ñ ïëàöåáî äâóñòîðîííèìè òåñòàìè ñ óðîâíåì äîñòîâåðíîñòè 0,05. Èçìåíåíèå ïàðàìåòðîâ áåçîïàñíîñòè ñ áàçîâûõ çíà÷åíèé îöåíèâàëîñü áåç ïîïðàâêè íà èñõîäíûå ïîêàçàòåëè, öåíòð èññëåäîâàíèÿ èëè äðóãèå ïåðåìåííûå. Êîëè÷åñòâî ïàöèåíòîâ ñî çíà÷èìûì óâåëè÷åíèåì ìàññû òåëà îöåíèâàëîñü ñ ïîìîùüþ òåñòà Cochran-Mantel-Haenzel. Êðèòåðèè âêëþ÷åíèÿ è èñêëþ÷åíèÿ  èññëåäîâàíèå áûëè âêëþ÷åíû áîëüíûå â âîçðàñòå îò 18 äî 65 ëåò ñ äèàãíîçîì øèçîôðåíèè èëè øèçîàôôåêòèâíîãî ðàññòðîéñòâà (DSM-IV), ãîñïèòàëèçèðîâàííûå â ñâÿçè ñ îáîñòðåíèåì çàáîëåâàíèÿ. Ïàöèåíòû äîëæíû áûëè èìåòü àíàìíåç óñïåøíîé àíòèïñèõîòè÷åñêîé òåðàïèè (îòñóòñòâèå ðåçèñòåíòíîñòè) è íàõîäèòüñÿ íà àìáóëàòîðíîì íàáëþäåíèè â òå÷åíèå ìèíèìóì 3-õ ìåñÿöåâ çà òåêóùèé ãîä; ñóììàðíûé áàëë ïî øêàëå ïîçèòèâíûõ è íåãàòèâíûõ ñèìïòîìîâ (PANSS) äîëæåí áûë ñîñòàâëÿòü íå ìåíåå 60, ïðè ýòîì, ïî ìåíüøåé ìåðå, 2 ïóíêòà ðàçäåëà ïîçèòèâíûõ ñèìïòîìîâ äîëæíû áûëè ñîîòâåòñòâîâàòü 4 áàëëàì (óìåðåííàÿ ñòåïåíü). Êðèòåðèè èñêëþ÷åíèÿ: àãðåññèâíûå äåéñòâèÿ â àíàìíåçå; íåäàâíèå ñóèöèäàëüíûå ïîïûòêè èëè íàëè÷èå ñåðüåçíûõ ñóèöèäàëüíûõ ìûñëåé; òÿæ¸ëàÿ íåâðîëîãè÷åñêàÿ ïàòîëîãèÿ, çà èñêëþ÷åíèåì ïîçäíåé äèñêèíåçèè èëè äðóãèõ ýêñòðàïèðàìèäíûõ ïîáî÷íûõ ÿâëåíèé; íàëè÷èå çàâèñèìîñòè îò ïñèõîàêòèâíûõ âåùåñòâ; äðóãàÿ îñòðàÿ ñîìàòè÷åñêàÿ ïàòîëîãèÿ. Äèçàéí èññëåäîâàíèÿ Äàííîå ðàíäîìèçèðîâàííîå, 4-íåäåëüíîå, ñòàöèîíàðíîå, äâîéíîå ñëåïîå ïëàöåáî-êîíòðîëèðóåìîå èññëåäîâàíèå ñ ïàðàëëåëüíûìè ãðóïïàìè, áûëî ïðîâåäåíî â 40 ìåäèöèíñêèõ öåíòðàõ â ÑØÀ â ïåðèîä ñ ñåíòÿáðÿ 1997 ãîäà ïî îêòÿáðü 1998 ãîäà. Ïàöèåíòû, ñîîòâåòñòâîâàâøèå êðèòåðèÿì âêëþ÷åíèÿ, ïðîõîäèëè ìèíèìóì 5-äíåâíûé ïåðèîä «îòìûâàíèÿ» (washout) ñ íàçíà÷åíèåì ïëàöåáî â òå÷åíèå ïåðâîé ñêðèíèíãîâîé íåäåëè. Ïàöèåíòû áûëè ðàñïðåäåëåíû ñëó÷àéíûì îáðàçîì â 4 ãðóïïû, êîòîðûå äîëæíû áûëè ïîëó÷àòü â òå÷åíèå 4 íåäåëü îäèí èç ñëåäóþùèõ ïðåïàðàòîâ – àðèïèïðàçîë 20 ìã/ñóò, àðèïèïðàçîë 30 ìã/ñóò, ðèñïåðèäîí 6 ìã/ñóò èëè ïëàöåáî. Ðèñïåðèäîí íàçíà÷àëñÿ ïåðîðàëüíî 2 ðàçà â äåíü ñ ïîñòåïåííûì ïîâûøåíèåì äîçû (2 ìã â ïåðâûé äåíü, 4 ìã âî âòîðîé äåíü è 6 ìã/ñóò â òå÷åíèå ïîñëåäóþùåãî ïåðèîäà). Àðèïèïðàçîë íàçíà÷àëñÿ â ïîëíîé ñóòî÷íîé äîçèðîâêå ïîñëå çàâòðàêà; âå÷åðîì ïàöèåíòû ïðèíèìàëè ïëàöåáî äëÿ ïîääåðæàíèÿ èññëåäîâàíèÿ ñëåïûì.  ãðóïïå ïëàöåáî, ïàöèåíòû ïðèíèìàëè åãî äâàæäû â äåíü, óòðîì è âå÷åðîì. Äîçèðîâêè ïðåïàðàòîâ áûëè ôèêñèðîâàííûìè è íå ìîãëè áûòü èçìåíåíû â ñâÿçè ñ íåäîñòàòî÷íîñòüþ ýôôåêòèâíîñòè èëè ðàçâèòèåì ïîáî÷íûõ ýôôåêòîâ. Îöåíêà ýôôåêòèâíîñòè. Òåðàïåâòè÷åñêàÿ ýôôåêòèâíîñòü îöåíèâàëàñü ñ ïîìîùüþ øêàë PANSS è Îáùåãî êëèíè÷åñêîãî âïå÷àòëåíèÿ (CGI). Îöåíêó ýôôåêòèâíîñòè ïðîâîäèëè íà ýòàïå ñêðèíèíãà, â êîíöå ïåðèîäà «îòìûâàíèÿ» (èñõîäíîå çíà÷åíèå) è ïîñëå çàâåðøåíèÿ êàæäîé íåäåëè ëå÷åíèÿ (äåíü 7, 14, 21 è 28). Îöåíèâàëèñü äèíàìèêà ïîêàçàòåëåé ïî øêàëå PANSS (â öåëîì, ïðîäóêòèâíàÿ è íåãàòèâíàÿ ñèìïòîìàòèêà) è CGI-S 73 Äåìîãðàôè÷åñêàÿ õàðàêòåðèñòèêà ïàöèåíòîâ  îáùåé ñëîæíîñòè 404 ïàöèåíòà (283 ìóæ. è 121 æåí.) áûëè ðàíäîìèçèðîâàíû â 4 òåðàïåâòè÷åñêèå ãðóïïû íà ïåðèîä â 4 íåäåëè: àðèïèïðàçîë 20 ìã/ñóò (n=101), àðèïèïðàçîë 30 ìã/ñóò (n=101), ðèñïåðèäîí 6 ìã/ñóò (n=99), ïëàöåáî (n=103). Ñðåäíèé âîçðàñò â êàæäîé ãðóïïå ñîñòàâèë îò 38,1 äî 40,2 ëåò. Ó 289 (72%) ïàöèåíòîâ áûë óñòàíîâëåí äèàãíîç øèçîôðåíèè, ó 115 (28%) – øèçîàôôåêòèâíîãî ðàññòðîéñòâà.  íà÷àëå èññëåäîâàíèÿ ñðåäíåå êîëè÷åñòâî áàëëîâ äëÿ âñåõ òåðàïåâòè÷åñêèõ ãðóïï ïî øêàëå PANSS ñîñòàâëÿëî îò 92,6 äî 95,7. Ñðåäíåå çíà÷åíèå âåñà òåëà ñîñòàâèëî 82,4–87,2 êã; ñðåäíåå ÷èñëî ãîñïèòàëèçàöèé – 8,6.  öåëîì, 242 (60%) ïàöèåíòà çàâåðøèëè èññëåäîâàíèå, 162 ïàöèåíòà ïðåæäåâðåìåííî ïðåêðàòèëè ïðè¸ì òåðàïèè. 42 (10%) èç 404 ïàöèåíòîâ ïðåêðàòèëè òåðàïèþ â ñâÿçè ñ îòñóòñòâèåì ïîëîæèòåëüíîãî òåðàïåâòè÷åñêîãî îòâåòà èëè óõóäøåíèåì ñèìïòîìàòèêè, 50 (12%) ïðåêðàòèëè ïðè¸ì òåðàïèè ïî ëè÷íûì ïðè÷èíàì è 44 (11%) – â ñâÿçè ñ ðàçâèòèåì íåæåëàòåëüíûõ ýôôåêòîâ. Íàèáîëüøåå ÷èñëî ïàöèåíòîâ, ïðåæäåâðåìåííî ïðåêðàòèâøèõ òåðàïèþ, îêàçàëîñü â ãðóïïå ïëàöåáî (n=51; 50%) è áûëî ñõîæèì â îñòàëüíûõ òð¸õ ãðóïïàõ (àðèïèïðàçîë 20 ìã, n=40, 40%; àðèïèïðàçîë 30 ìã, n=34, 34%; ðèñïåðèäîí, n=37, 37%). Арипипразол 30 мг Рисперидон 6 мг Средний показатель из менения общего показа теля подшкалы негатив ных симптомов PANSS от начала лечения Средний показатель из менения общего показа теля подшкалы позитив ных симптомов PANSS от начала лечения Средний показатель изменения общего по казателя шкалы PANSS от начала лечения Плацебо Арипипразол 20 мг Ýôôåêòèâíîñòü  ñðàâíåíèè ñ ïëàöåáî â îáåèõ ãðóïïàõ ñ àðèïèïðàçîëîì áûëî äîñòèãíóòî äîñòîâåðíî çíà÷èìîå óëó÷øåíèå ïî 3 îñíîâíûì êðèòåðèÿì: îáùàÿ îöåíêà ïî øêàëå PANSS (àðèïèïðàçîë 20 ìã, p=0,001; àðèïèïðàçîë 30 ìã, p=0,003), îöåíêà ïî ïîäøêàëå ïîçèòèâíûõ ñèìïòîìîâ PANSS (àðèïèïðàçîë 20 ìã, p=0,001; àðèïèïðàçîë 30 ìã, p=0,02) è CGI-S (àðèïèïðàçîë 20 ìã, p=0,03; àðèïèïðàçîë 30 ìã, p=0,006).  ãðóïïå ðèñïåðèäîíà òàêæå áûëî îòìå÷åíî äîñòîâåðíî áîëüøåå óëó÷øåíèå ïî âñåì ïîêàçàòåëÿì ýôôåêòèâíîñòè (òàáëèöà). Îòìå÷àëîñü áûñòðîå äîñòèæåíèå ýôôåêòà (ðèñóíîê). Ñðåäíèé ïîêàçàòåëü èçìåíåíèÿ îáùåãî áàëëà ïî øêàëå PANSS (À), ïîäøêàëû ïîçèòèâíûõ (Â) è íåãàòèâíûõ (Ñ) ñèìïòîìîâ îò íà÷àëà ëå÷åíèÿ äî 4 íåä ëå÷åíèÿ àðèïèïðàçîëîì (20 èëè 30 ìã/ñóò), ðèñïåðèäîíîì (6 ìã/ñóò) èëè ïëàöåáî (ìåòîä ïåðåíîñà ïîñëåäíåãî èçìåðåíèÿ âïåðåä – LOCF) Ïðèìå÷àíèÿ: * – p<0,05 â ñðàâíåíèè ñ ïëàöåáî; † – p<0,01 â ñðàâíåíèè ñ ïëàöåáî; ‡ – p≤0,001 â ñðàâíåíèè ñ ïëàöåáî. Показатели эффективности: изменение показателей от исходного уровня до последней оценки состояния (метод LOCF) Ïàðàìåòð Ïëàöåáî Àðèïèïðàçîë Çíà÷åíèå p vs Àðèïèïðàçîë Çíà÷åíèå p vs Ðèñïåðèäîí Çíà÷åíèå p vs (n=103) 20 ìã (n=98) ïëàöåáî 30 ìã (n=96) ïëàöåáî 6 ìã (n=95) ïëàöåáî Ñðåäíåå çíà÷åíèå áàëëîâ ïî PANSS Îáùåå çíà÷åíèå -5,0 -14,5 0,001 -13,9 0,003 -15,7 <0,001 Ïîçèòèâíûå ñèìïòîìû -1,8 -4,9 0,001 -3,9 0,02 -5,2 <0,001 Íåãàòèâíûå ñèìïòîìû -0,8 -3,4 0,002 -3,4 0,002 -3,1 0,005 Øêàëà BPRS -1,7 -3,5 0,004 -3,3 0,01 -3,9 <0,001 Øêàëà CGI-S -0,2 -0,5 0,3 -0,6 0,006 -0,7 <0,001 Ñðåäíåå çíà÷åíèå ïî øêàëå CGI-I* 4,0 3,4 0,005 3,3 0,001 3,3 <0,001 24 (23) 35 (36) 0,04 39 (41) 0,005 38 (40) 0,008 Óðîâåíü ðåñïîíäåðîâ, êîëè÷åñòâî (%)** Ïðèìå÷àíèÿ: BPRS – êðàòêàÿ øêàëà ïñèõèàòðè÷åñêîé îöåíêè, CGI-I – øêàëà îáùåãî êëèíè÷åñêîãî âïå÷àòëåíèÿ, ïîäøêàëà «Óëó÷øåíèå», CGI-S – øêàëà îáùåãî êëèíè÷åñêîãî âïå÷àòëåíèÿ, ïîäøêàëà «Òÿæåñòü çàáîëåâàíèÿ», PANSS – øêàëà ïîçèòèâíûõ è íåãàòèâíûõ ñèìïòîìîâ. * – çíà÷åíèÿ ïðèâåäåíû êàê ñðåäíèå äàííûå èçìåíåíèé èñõîäíûõ âåëè÷èí. ** – ïàöèåíòû ñ 30% èëè áîëüøèì ñíèæåíèåì çíà÷åíèé ïî øêàëå PANSS èëè ñî çíà÷åíèåì 1 (çíà÷èòåëüíîå óëó÷øåíèå) èëè 2 (óëó÷øåíèå) ïî øêàëå CGI-I. 74 Áûëî âûÿâëåíî äîñòîâåðíîå ïðåèìóùåñòâî àðèïèïðàçîëà (20 ìã è 30 ìã) â ñðàâíåíèè ñ ïëàöåáî ïî øêàëå CGI-I (àðèïèïðàçîë 20 ìã, p=0,002; àðèïèïðàçîë 30 ìã, p=0,001) (ðèñóíîê) è øêàëå BPRS (àðèïèïðàçîë 20 ìã, p=0,004; àðèïèïðàçîë 30 ìã, p=0,01) (òàáëèöà).  îòíîøåíèè âñåõ òð¸õ ïàðàìåòðîâ ñòàòèñòè÷åñêè äîñòîâåðíûå ðàçëè÷èÿ â ãðóïïàõ ñ àðèïèïðàçîëîì è ïëàöåáî ñòàëè îáíàðóæèâàòüñÿ ñ 1-é íåäåëè òåðàïèè. Ñòàòèñòè÷åñêè äîñòîâåðíûå ðàçëè÷èÿ ìåæäó ðèñïåðèäîíîì è ïëàöåáî áûëè îòìå÷åíû ñî 2-é íåäåëè ïî ðàçäåëó íåãàòèâíûå ñèìïòîìû øêàëû PANSS (ðèñóíîê) è ñ ïåðâîé íåäåëè ïî øêàëå CGI-I è BPRS. Êîëè÷åñòâî ðåñïîíäåðîâ ïî øêàëàì PANSS è CGI-I áûëî äîñòîâåðíî áîëüøå â îáåèõ ãðóïïàõ àðèïèïðàçîëà â ñðàâíåíèè ñ ãðóïïîé ïëàöåáî (ïëàöåáî – 23%; àðèïèïðàçîë 20 ìã – 36%, p=0,04; àðèïèïðàçîë 30 ìã, p=0,005).  ãðóïïå ðèñïåðèäîíà òàêæå áûëî äîñòîâåðíî áîëüøå ðåñïîíäåðîâ â ñðàâíåíèè ñ ãðóïïîé ïëàöåáî (40%; p=0,008) (òàáëèöà). ñîîáùàëîñü îá ýêñòðàïèðàìèäíûõ ïîáî÷íûõ ýôôåêòàõ. Äèñòîíèÿ/ãèïåðòîíóñ áûëè îòìå÷åíû ó 14 (14%) ïàöèåíòîâ â ãðóïïå ðèñïåðèäîíà â ñðàâíåíèè ñ 3 (3%) ïàöèåíòàìè â ãðóïïå àðèïèïðàçîëà 20 ìã, 1 (1%) â ãðóïïå àðèïèïðàçîëà 30 ìã è 6 (6%) â ãðóïïå ïëàöåáî. Îöåíêà ïî øêàëå Ñèìïñîí-Àíãóñà: ñðåäíåå çíà÷åíèå èçìåíåíèé ïîêàçàòåëåé îò èñõîäíîãî óðîâíÿ â ãðóïïå àðèïèïðàçîëà 20 ìã ñîñòàâèëî -0,16; -0,09 â ãðóïïå àðèïèïðàçîëà 30 ìã; -0,18 â ãðóïïå ðèñïåðèäîíà è -0,18 â ãðóïïå ïëàöåáî. Ïîïàðíîå ñðàâíåíèå íå âûÿâèëî ñòàòèñòè÷åñêè çíà÷èìûõ ðàçëè÷èé ìåæäó ãðóïïàìè ñ àêòèâíîé òåðàïèåé è ïëàöåáî. Îáùåå ÷èñëî áàëëîâ ïî øêàëå àêàòèçèè Áàðíñà: ñðåäíåå çíà÷åíèå èçìåíåíèé ïîêàçàòåëåé îò èñõîäíîãî óðîâíÿ â ãðóïïå àðèïèïðàçîëà 20 ìã ñîñòàâèëî -0,15; -0,18 â ãðóïïå àðèïèïðàçîë 30 ìã; 0,14 â ãðóïïå ðèñïåðèäîíà è 0,11 â ãðóïïå ïëàöåáî. Ïîïàðíîå ñðàâíåíèå íå âûÿâèëî ñòàòèñòè÷åñêè çíà÷èìûõ ðàçëè÷èé ìåæäó ãðóïïàìè ñ àêòèâíîé òåðàïèåé è ïëàöåáî. Øêàëà îöåíêè ïàòîëîãè÷åñêèõ íåïðîèçâîëüíûõ äâèæåíèé: ñðåäíåå çíà÷åíèå èçìåíåíèé ïîêàçàòåëåé îò èñõîäíîãî óðîâíÿ â ãðóïïå àðèïèïðàçîëà 20 ìã ñîñòàâèëî -0,27; -0,5 â ãðóïïå àðèïèïðàçîëà 30 ìã; -0,6 â ãðóïïå ðèñïåðèäîíà è 0,1 â ãðóïïå ïëàöåáî.  ñðàâíåíèè ñ ïëàöåáî, ðèñïåðèäîí ïðîäåìîíñòðèðîâàë ñòàòèñòè÷åñêè çíà÷èìûå ðàçëè÷èÿ (p=0,03). Äàííûå îá èñïîëüçîâàíèè áåíçòðîïèíà áûëè ñõîæèìè âî âñåõ òð¸õ ãðóïïàõ àêòèâíîé òåðàïèè. Ìàññà òåëà. Èçìåðåíèå ìàññû òåëà çà ïåðèîä èññëåäîâàíèÿ ïîêàçàëî ìèíèìàëüíîå óâåëè÷åíèå çíà÷åíèé ñ èñõîäíûõ ïîêàçàòåëåé â äèíàìèêå âî âñåõ òð¸õ ãðóïïàõ òåðàïèè: àðèïèïðàçîë 20 ìã – 1,2 êã, àðèïèïðàçîë 30 ìã – 0,8 êã, ðèñïåðèäîí 6 ìã – 1,5 êã. Ýòè çíà÷åíèÿ ñòàòèñòè÷åñêè çíà÷èìî îòëè÷àëèñü îò ïîêàçàòåëåé â ãðóïïå ïëàöåáî, â êîòîðîé áûëî îòìå÷åíî ñíèæåíèå ìàññû òåëà çà ïåðèîä èññëåäîâàíèÿ íà 0,3 êã. ×àñòîòà êëèíè÷åñêè çíà÷èìîé ïðèáàâêè ìàññû òåëà (ïîâûøåíèå ìàññû òåëà íà ≥7% îò èñõîäíûõ ïîêàçàòåëåé) îêàçàëàñü äîñòîâåðíî âûøå íà ôîíå âñåõ âàðèàíòîâ òåðàïèè â ñðàâíåíèè ñ ïëàöåáî: ïëàöåáî – 2%; àðèïèïðàçîë 20 ìã – 13% (p=0,004); àðèïèïðàçîë 30 ìã – 9% (p=0,04); ðèñïåðèäîí 6 ìã – 11% (p=0,03). Óðîâåíü ïðîëàêòèíà â ïëàçìå êðîâè. Çà ïåðèîä èññëåäîâàíèÿ áûëî îòìå÷åíî ñíèæåíèå óðîâíÿ ïðîëàêòèíà â ïëàçìå êðîâè ñ èñõîäíûõ çíà÷åíèé â îáåèõ ãðóïïàõ àðèïèïðàçîëà (àðèïèïðàçîë 20 ìã, -6,6 íã/ìë; àðèïèïðàçîë 30 ìã, -6,4 íã/ìë) è ïîâûøåíèå â ãðóïïå ïëàöåáî (0,1 íã/ìë); ðàçëè÷èÿ ìåæäó ãðóïïàìè àðèïèïðàçîëà è ïëàöåáî íå äîñòèãàëè ñòàòè÷åñêè çíà÷èìûõ çíà÷åíèé. Íè ó îäíîãî èç ïàöèåíòîâ, ïîëó÷àâøèõ àðèïèïðàçîë, óðîâåíü ïðîëàêòèíà â ïëàçìå êðîâè íå áûë íèæå íèæíåé ãðàíèöû ðåôåðåíòíûõ çíà÷åíèé (2 íã/ìë).  ãðóïïå ðèñïåðèäîíà îòìå÷àëîñü ïîâûøåíèå óðîâíÿ ïðîëàêòèíà â êðîâè äî 47,9 íã/ìë, ÷òî áûëî äîñòîâåðíî âûøå, Áåçîïàñíîñòü Íåæåëàòåëüíûå ÿâëåíèÿ.  öåëîì, òåðàïèÿ àðèïèïðàçîëîì â îáåèõ äîçèðîâêàõ õîðîøî ïåðåíîñèëàñü ïàöèåíòàìè è áûëà áåçîïàñíîé. Áîëüøèíñòâî âîçíèêàâøèõ íåæåëàòåëüíûõ ÿâëåíèé áûëî âûðàæåíî â ë¸ãêîé èëè óìåðåííîé ñòåïåíè è, â îñíîâíîì, íå îãðàíè÷èâàëî òåðàïèþ.  îáùåé ñëîæíîñòè 44 (11%) èç 403 ïàöèåíòîâ âûáûëè èç èññëåäîâàíèÿ â ñâÿçè ñ íåæåëàòåëüíûìè ÿâëåíèÿìè íà ôîíå ëå÷åíèÿ: 17 (17%) â ãðóïïå ïëàöåáî, 8 (8%) â ãðóïïå ðèñïåðèäîíà, 11 (11%) â ãðóïïå àðèïèïðàçîëà 20 ìã è 8 (8%) â ãðóïïå àðèïèïðàçîëà 30 ìã. ×àùå âñåãî òåðàïèÿ ïðåêðàùàëàñü â ñâÿçè ñ ðàçâèòèåì ïñèõîòè÷åñêîãî ñîñòîÿíèÿ: 8 (8%) â ãðóïïå ïëàöåáî, 5 (5%) â ãðóïïå ðèñïåðèäîíà, 10 (10%) ïàöèåíòîâ â ãðóïïå àðèïèïðàçîëà 20 ìã è 5 (5%) ïàöèåíòîâ â ãðóïïå àðèïèïðàçîëà 30 ìã. Êîëè÷åñòâî ïàöèåíòîâ, èñïûòàâøèõ íåæåëàòåëüíûå ÿâëåíèÿ â ñâÿçè ñ òåðàïèåé, áûëî ïðèìåðíî îäèíàêîâûì âî âñåõ òåðàïåâòè÷åñêèõ ãðóïïàõ: 91% (92 ÷åë.) â ãðóïïå àðèïèïðàçîëà 20 ìã, 91% (91 ÷åë.) â ãðóïïå àðèïèïðàçîëà 30 ìã, 93% (92 ÷åë.) â ãðóïïå ðèñïåðèäîíà è 86% (89 ÷åë.) â ãðóïïå ïëàöåáî. Ó ïàöèåíòîâ, ïîëó÷àâøèõ àðèïèïðàçîë, òàêèå íåæåëàòåëüíûå ÿâëåíèÿ êàê ãîëîâíàÿ áîëü, òîøíîòà, ðâîòà, áåññîííèöà, ñîìíîëåíöèÿ, âîçíèêàëè â îñíîâíîì â òå÷åíèå ïåðâîé íåäåëè òåðàïèè è ñîõðàíÿëèñü íå áîëåå 7 äíåé. Íå ïðîñëåæèâàëîñü äîçîçàâèñèìîå âîçíèêíîâåíèå íåæåëàòåëüíûõ ÿâëåíèé, âîçìîæíî, çà èñêëþ÷åíèåì ñîìíîëåíöèè. Çà ïåðèîä èññëåäîâàíèÿ, â öåëîì, ó 8 ïàöèåíòîâ áûëî îòìå÷åíî ðàçâèòèå ñåðüåçíûõ íåæåëàòåëüíûõ ÿâëåíèé (àðèïèïðàçîë 20 ìã, n=2; àðèïèïðàçîë 30 ìã, n=3; ïëàöåáî, n=3). Ýêñòðàïèðàìèäíûå ñèìïòîìû.  öåëîì, ÷àñòîòà âîçíèêíîâåíèÿ ÝÏÑ áûëà ñõîæåé â ãðóïïå àðèïèïðàçîëà è ðèñïåðèäîíà (àðèïèïðàçîë 20 ìã, n=32, 32%; àðèïèïðàçîë 30 ìã, n=31, 31%; ðèñïåðèäîí, n=31, 31%).  ãðóïïå ïëàöåáî ó 21 (20%) ïàöèåíòà 75 ÷åì â ãðóïïå ïëàöåáî (p<0,001). Êîëè÷åñòâî ïàöèåíòîâ ñ óðîâíåì ïðîëàêòèíà â ïëàçìå êðîâè âûøå 23 íã/ìë (âåðõíÿÿ ãðàíèöà ðåôåðåíòíûõ çíà÷åíèé) ñîñòàâèëî â ãðóïïå ïëàöåáî 10,3%; â ãðóïïå àðèïèïðàçîëà 20 ìã – 4,1% (p=0,16 vs ïëàöåáî); àðèïèïðàçîë 30 ìã – 3,3% (p=0,08 vs ïëàöåáî) è â ãðóïïå ðèñïåðèäîíà – 90,5% (p<0,001 vs ïëàöåáî). Ýëåêòðîêàðäèîãðàììà. Èíòåðâàë QTc ðàññ÷èòûâàëñÿ ñ ïîìîùüþ ôîðìóëû Áàçåòòà (QTcB=QT/RR0,5). Ñðåäíèå çíà÷åíèÿ äèíàìèêè èíòåðâàëà QT c äëÿ êàæäîé òåðàïåâòè÷åñêîé ãðóïïû ñîñòàâèëè: àðèïèïðàçîë 20 ìã, 0,97 ìèëëèñåêóíä; àðèïèïðàçîë 30 ìã, -2,35 ìèëëèñåêóíä; ïëàöåáî, -2,18 ìèëëèñåêóíä; ðèñïåðèäîí, 6,31 ìèëëèñåêóíäó. Íè ó îäíîãî èç ïàöèåíòîâ, ïîëó÷àâøèõ àðèïèïðàçîë èëè ïëàöåáî, íå áûëî îòìå÷åíî êëèíè÷åñêè çíà÷èìîãî óâåëè÷åíèÿ èíòåðâàëà QTc (êëèíè÷åñêè çíà÷èìûì ñ÷èòàëîñü óâåëè÷åíèå äî 450 ìèëëèñåêóíä èëè áîëåå, à òàêæå óâåëè÷åíèå ïîêàçàòåëÿ íà 10% èëè áîëåå ñ èñõîäíûõ çíà÷åíèé); â ãðóïïå ðèñïåðèäîíà ïîäîáíûå îòêëîíåíèÿ íàáëþäàëèñü ó 3 (3%) èç 95 áîëüíûõ. Î÷åâèäíûõ ðàçëè÷èé ìåæäó òåðàïåâòè÷åñêèìè ãðóïïàìè ïî ÷àñòîòå âîçíèêíîâåíèÿ êëèíè÷åñêè çíà÷èìûõ îòêëîíåíèé ëàáîðàòîðíûõ è âèòàëüíûõ ïîêàçàòåëåé îòìå÷åíî íå áûëî, íè îäèí èç ïàöèåíòîâ íå âûáûë èç èññëåäîâàíèÿ â ñâÿçè ñ ïàòîëîãè÷åñêèìè èçìåíåíèÿìè æèçíåííî âàæíûõ ïîêàçàòåëåé. Íå áûëî âûÿâëåíî êëèíè÷åñêè çíà÷èìîé ðàçíèöû â ëàáîðàòîðíûõ ïîêàçàòåëÿõ ìåæäó ãðóïïàìè, çà èñêëþ÷åíèåì çíà÷åíèé óðîâíÿ ïðîëàêòèíà â ïëàçìå êðîâè. Îäèí ïàöèåíò â ãðóïïå ðèñïåðèäîíà âûáûë èç èññëåäîâàíèÿ â ñâÿçè ñ óìåðåííûìè èçìåíåíèÿìè ïîêàçàòåëåé ôóíêöèè ïå÷åíè. ïè÷íûõ àíòèïñèõîòèêîâ (3, 5, 7, 24, 26, 34). Òåðàïèÿ àðèïèïðàçîëîì â îáåèõ äîçèðîâêàõ õîðîøî ïåðåíîñèëàñü.  äàííîé ðàáîòå è â ðàíåå ïðîâåä¸ííûõ èññëåäîâàíèÿõ àðèïèïðàçîëà (9, 15) íå îòìå÷àëîñü çàâèñèìîñòè âîçíèêíîâåíèÿ ïîáî÷íûõ ýôôåêòîâ îò äîçèðîâêè ïðåïàðàòà, çà èñêëþ÷åíèåì ñîìíîëåíöèè. Âûðàæåííîñòü ýêñòðàïèðàìèäíîé ñèìïòîìàòèêè íå îòëè÷àëàñü â ãðóïïàõ àðèïèïðàçîëà ïî ñðàâíåíèþ ñ ïëàöåáî, ÷òî ñîîòâåòñòâóåò äàííûì êëèíè÷åñêîé ïðîãðàììû ïî èçó÷åíèþ àðèïèïðàçîëà (22).  ãðóïïå ðèñïåðèäîíà ÷àùå áûëè îòìå÷åíû äèñòîíèÿ/ãèïåðòîíóñ. Ýòî ìîæåò áûòü ñâÿçàíî ñ òåì, ÷òî ðèñïåðèäîí â äîçèðîâêå 6 ìã/ñóò îáëàäàåò ñïîñîáíîñòüþ âûçûâàòü ðàçâèòèå ÝÏÑ. Çíà÷èòåëüíîå ïîâûøåíèå óðîâíÿ ïðîëàêòèíà â êðîâè è âûñîêàÿ ÷àñòîòà ðàçâèòèÿ ãèïåðïðîëàêòèíåìèè íà ïðîòÿæåíèè âñåãî èññëåäîâàíèÿ îòìå÷àëàñü â ãðóïïå ðèñïåðèäîíà. Íè â îäíîé èç ãðóïï àðèïèïðàçîëà íå áûëî îòìå÷åíî ñòàòèñòè÷åñêè çíà÷èìîãî óâåëè÷åíèÿ óðîâíÿ ïðîëàêòèíà â ïëàçìå êðîâè, íàïðîòèâ, â îáåèõ ãðóïïàõ áûëî çàôèêñèðîâàíî íåêîòîðîå ñíèæåíèå ýòîãî ïîêàçàòåëÿ îò èñõîäíûõ çíà÷åíèé. Ïîâûøåíèå óðîâíÿ ïðîëàêòèíà â ïëàçìå êðîâè âûøå âåðõíåé ãðàíèöû ðåôåðåíòíûõ çíà÷åíèé áûëî îòìå÷åíî ó 10,3% ïàöèåíòîâ â ãðóïïå ïëàöåáî, 4,1% è 3,3% â ãðóïïàõ àðèïèïðàçîëà 20 ìã è 30 ìã ñîîòâåòñòâåííî è â 90,5% ñëó÷àåâ â ãðóïïå ðèñïåðèäîíà. Òàê êàê äîôàìèí èíãèáèðóåò âûñâîáîæäåíèå ïðîëàêòèíà, íåêîòîðîå ñíèæåíèå óðîâíÿ ïðîëàêòèíà ïðè íàçíà÷åíèè àðèïèïðàçîëà ìîæåò áûòü îáúÿñíåíî ÷àñòè÷íûì àãîíèçìîì äîôàìèíîâûõ ðåöåïòîðîâ, ÷òî îòðàæàåò äàííûå ïðåêëèíè÷åñêèõ èññëåäîâàíèé (13). Ïðè ïðèåìå íåêîòîðûõ àíòèïñèõîòè÷åñêèõ ñðåäñòâ îòìå÷åíî óäëèíåíèå èíòåðâàëà QTc íà ÝÊà (12), ÷òî ìîæåò áûòü ïðè÷èíîé ðàçâèòèÿ ëåòàëüíîé ñåðäå÷íîé àðèòìèè. Ó òðåõ ïàöèåíòîâ â ãðóïïå ðèñïåðèäîíà áûëî îòìå÷åíî êëèíè÷åñêè çíà÷èìîå óäëèíåíèå èíòåðâàëà QTc; îòñóòñòâèå ñëó÷àåâ óäëèíåíèÿ èíòåðâàëà QTc â îáåèõ ãðóïïàõ àðèïèïðàçîëà ïîäòâåðæäàåò íèçêèé óðîâåíü àðèòìîãåííîãî äåéñòâèÿ äàííîãî ïðåïàðàòà. Çíà÷èòåëüíûé èíòåðåñ âûçûâàåò ïðîáëåìà ïîâûøåíèÿ ìàññû òåëà íà ôîíå ïðèåìà àíòèïñèõîòè÷åñêîé òåðàïèè (1, 2). Óâåëè÷åíèå ìàññû òåëà ìîæåò ÿâèòüñÿ ïðè÷èíîé ðàçâèòèÿ ñåðäå÷íî-ñîñóäèñòûõ îñëîæíåíèé è ñàõàðíîãî äèàáåòà, à òàêæå ìîæåò ïðèâîäèòü ê íèçêîé êîìïëàéåíòíîñòè ïàöèåíòà.  íàñòîÿùåì èññëåäîâàíèè êîëè÷åñòâî ïàöèåíòîâ ñ êëèíè÷åñêè çíà÷èìîé ïðèáàâêîé ìàññû òåëà áûëî ïðèìåðíî îäèíàêîâûì âî âñåõ 3 ãðóïïàõ òåðàïèè (9–13%).  õîäå íàñòîÿùåãî êðàòêîñðî÷íîãî èññëåäîâàíèÿ ñðåäíèå ïîêàçàòåëè èçìåíåíèÿ ìàññû òåëà (0,8–1,5 êã) íå áûëè êëèíè÷åñêè çíà÷èìûìè. Äëÿ îöåíêè äèíàìèêè ïîâûøåíèÿ ìàññû òåëà è åå ïîñëåäñòâèé íåîáõîäèì áîëåå äëèòåëüíûé ïåðèîä íàáëþäåíèÿ. Ðåçóëüòàòû íàñòîÿùåãî èññëåäîâàíèÿ ñâèäåòåëüñòâóþò î òîì, ÷òî àðèïèïðàçîë îáëàäàåò ýôôåêòèâ- Êîììåíòàðèè  äàííîì èññëåäîâàíèè áûëî ïîêàçàíî, ÷òî àðèïèïðàçîë â äîçèðîâêå 20 è 30 ìã/ñóò ÿâëÿåòñÿ ýôôåêòèâíûì, áåçîïàñíûì è õîðîøî ïåðåíîñèìûì ïðåïàðàòîì äëÿ òåðàïèè ïàöèåíòîâ ñ îáîñòðåíèåì øèçîôðåíèè èëè øèçîàôôåêòèâíîãî ðàññòðîéñòâà. Áûëî âûÿâëåíî äîñòîâåðíîå ïðåèìóùåñòâî àðèïèïðàçîëà (20 è 30 ìã/ñóò) ïî ñðàâíåíèþ ñ ïëàöåáî ïî âñåì îñíîâíûì êðèòåðèÿì îöåíêè ýôôåêòèâíîñòè (îáùåå ÷èñëî áàëëîâ ïî øêàëå PANSS, áàëëû ïîçèòèâíîãî è íåãàòèâíîãî ðàçäåëîâ øêàëû PANSS, áàëëû ïî øêàëå CGI-S, ïî øêàëå BPRS, ñðåäíåå çíà÷åíèå ïî øêàëå CGI-I è âðåìÿ îòâåòà íà òåðàïèþ). Óëó÷øåíèå ñèìïòîìàòèêè íà òåðàïèè àðèïèïðàçîëîì áûëî ñðàâíèìûì ñ òàêîâûì íà òåðàïèè ðèñïåðèäîíîì. Áûñòðîå äîñòèæåíèå ýôôåêòà áûëî ïðîäåìîíñòðèðîâàíî â îáåèõ ãðóïïàõ àðèïèïðàçîëà: äîñòîâåðíî çíà÷èìîå êëèíè÷åñêîå óëó÷øåíèå â ñðàâíåíèè ñ ïëàöåáî îòìå÷àëîñü óæå íà ïåðâîé íåäåëå òåðàïèè, ñîõðàíÿÿñü äî êîíöà èññëåäîâàíèÿ.  ïðåäøåñòâóþùèõ ðàáîòàõ òàêæå áûëà ïîêàçàíà ýôôåêòèâíîñòü 15 ìã ïðåïàðàòà (28). ×àñòîòà äîñðî÷íîãî ïðåêðàùåíèÿ òåðàïèè â äàííîì èññëåäîâàíèè ñîîòâåòñòâóåò òàêîâîé äëÿ àòè76 íîñòüþ â îòíîøåíèè ëå÷åíèÿ ïñèõîòè÷åñêèõ ðàññòðîéñòâ ó áîëüíûõ øèçîôðåíèåé. Íåêîòîðûå îðèãèíàëüíûå äàííûå, îáíàðóæåííûå â õîäå íàñòîÿùåãî èññëåäîâàíèÿ, ìîãóò áûòü îáúÿñíåíû óíèêàëüíûì ìåõàíèçìîì äåéñòâèÿ àðèïèïðàçîëà, à èìåííî ÷àñòè÷íîé àãîíèñòè÷åñêîé àêòèâíîñòüþ ê D 2 , 5HT1A-ðåöåïòîðàì è àíòàãîíèñòè÷åñêîé àêòèâíîñòüþ â îòíîøåíèè 5HT2A-ðåöåïòîðîâ. Áûëî ïîêàçàíî, ÷òî àðèïèïðàçîë â äîçèðîâêå 20 ìã è 30 ìã ÿâëÿåòñÿ ýôôåêòèâíûì â îòíîøåíèè ïîçèòèâíûõ è íåãàòèâíûõ ñèìïòîìîâ øèçîôðåíèè. Òàêæå â íàñòîÿùåì èññëåäîâàíèè áûëî ïðîäåìîíñòðèðîâàíî áûñòðîå íà÷àëî äåéñòâèÿ àðèïèïðàçîëà è ñòàáèëüíîñòü ïîëîæèòåëüíîãî ýôôåêòà íà ïðîòÿæåíèè 4-õ íåäåëü èññëåäîâàíèÿ. Ýòè äàííûå ïîêàçûâàþò, ÷òî àðèïèïðàçîë – ïåðâûé ÷àñòè÷íûé àãîíèñò äîôàìèíà, îêàçûâàþùèé çíà÷èòåëüíîå è äëèòåëüíîå àíòèïñèõîòè÷åñêîå äåéñòâèå. Äîñòèæåíèå àíòèïñèõîòè÷åñêîãî ýôôåêòà íà ôîíå ïðèåìà àðèïèïðàçîëà â äîçèðîâêå 20 ìã è 30 ìã íå ñîïðîâîæäàëîñü ðàçâèòèåì òàêèõ íåæåëàòåëüíûõ ÿâëåíèé êàê óäëèíåíèå èíòåðâàëà QT c, çíà÷èìûõ ÝÏÑ èëè ïîâûøåíèÿ ìàññû òåëà. Íèçêèé ðèñê ðàçâèòèÿ ãèïåðïðîëàêòèíåìèè è ÝÏÑ íà ôîíå ïðèåìà àðèïèïðàçîëà, ïðîäåìîíñòðèðîâàííûé â äàííîì è ðÿäå ðàíåå ïðîâåäåííûõ èññëåäîâàíèé, îáúÿñíÿåòñÿ ÷àñòè÷íîé àãîíèñòè÷åñêîé àêòèâíîñòüþ â îòíîøåíèè D2-ðåöåïòîðîâ, â îòëè÷èå îò äðóãèõ äîñòóïíûõ â íàñòîÿùåå âðåìÿ àíòèïñèõîòèêîâ, áëîêèðóþùèõ D2-ðåöåïòîðû â íèãðîñòðèàðíîé è òóáåðîèíôóíäèáóëÿðíîé ñèñòåìàõ. Ñî÷åòàíèå äëèòåëüíîãî ïîëîæèòåëüíîãî ýôôåêòà è õîðîøåé ïåðåíîñèìîñòè ìîæåò ïîñëóæèòü óëó÷øåíèþ êîìïëàéåíñà ïàöèåíòîâ è ñíèçèòü ÷àñòîòó ðåöèäèâà çàáîëåâàíèÿ â äîëãîñðî÷íîé ïåðñïåêòèâå. Òàêèì îáðàçîì, ðåçóëüòàòû íàñòîÿùåãî èññëåäîâàíèÿ ñâèäåòåëüñòâóþò î òîì, ÷òî àðèïèïðàçîë îòêðûâàåò íîâûå âîçìîæíîñòè òåðàïèè øèçîôðåíèè è øèçîàôôåêòèâíîãî ðàññòðîéñòâà. ËÈÒÅÐÀÒÓÐÀ 16. Kapur S., Seeman P. Antipsychotic agents differ in how fast they come off the dopamine D2 receptors: implications for atypical antipsychotic action // J. Psychiatry Neurosci. – 2000. – Vol. 25. – P. 161– 166. 17. Kapur S., Seeman P. Does fast dissociation from the dopamine D2 receptor explain the action of atypical antipsychotics? a new hypothesis // Am. J. Psychiatry. – 2001. – Vol. 158. – P. 360–369. 18. Kikuchi T., Tottori K., Uwahodo Y. et al. 7-(4-[(2,3Dichlorophenyl)-1-piperazinyl]butyoxyl-3,4-dihydro-2 (IH)-quinolinone (OPC-14597), a new putative antipsychotic drug with both presynaptic and postsynaptic D2 receptor antagonist activity // J. Pharmacol. Exp. Ther. – 1995. – Vol. 274. – P. 329–336. 19. Kurzthaler I., Fleishhacker W.W. The clinical implications of weight gain in schizophrenia // J. Clin. Psychiatry. – 2001. – Vol. 62, Suppl. 7. – P. 32–37. 20. Lahti A.C., Weiler M.A., Corey P.K. et al. Antipsychotic properties of the partial dopamine agonist (-)-3-(3-hydroxyphenyl)-N-npropylpiperidine (preclamot) in schizophrenia // Biol. Psychiatry. – 1998. – Vol. 43. – P. 2–11. 21. Leysen J.E., Janssen P.M., Schotte A. et al. Interaction of antipsychotic drugs with neurotransmitter receptor sites in vitro and in vivo in relation to pharmacological and clinical effects: role of 5HT2 receptors // Psychopharmacol. – 1993. – Vol. 112, Suppl. 1. – P. S40–S54. 22. Marder S.R., McQuade R.D., Stock E. et al. Aripripazole in the treatment of schizophrenia: safety and tolerability in short-term, placebocontrolled trials // Schizophr. Res. – 2003. – Vol. 61. – P. 123–126. 23. McQuade R.D., Burris K.D., Jordan S. et al. Aripiprazole: a dopamine-serotonin system stabilizer [abstract] // Int. Neuropsychopharmacol. – 2002. – Vol. 5, Suppl. 1. – P. S176. 24. Meltzer H.Y., Stahl S.M. The dopamine hypothesis of schizophrenia: a review // Schizophr. Bull. – 1976. – Vol. 2. – P. 19–76. 25. Meltzer H.Y. The role of serotonin in antipsychotic drug action // Neuropsychopharmacology. – 1999. – Vol. 21, Suppl. 2. – P. 106S–115S. 26. Millan M.J. Improving the treatment of schizophrenia: focus on serotonin (5-HT1A) receptors // J. Pharmacol. Exp. Ther. – 2000. – Vol. 295. – P. 853–861. 27. Naber O., Gaussares C., Moeglen J.M, Tremmel L., Bailey P.E., and the SDZ HOC 912 Collaborative Study Group. Efficacy and tolerability of SDZ HOC 912, a partial dopamine D-2 agonist, in the treatment of schizophrenia // New Research Directions in the Development of Atypical and Other Novel Antipsychotic Medications / H.Y.Meltzer (Ed.). – New York, NY: Raven Press, 1991. 28. Olbrich R., Schanz H. An evaluation of the partial dopamine agonist terguride regarding positive symptoms reduction in schizophrenics // J. Neural Transm. Gen. Sect. – 1991. – Vol. 84. – P. 233–236. 29. Olbrich R., Schanz H. The effect of the partial dopamine agonist terguride on negative symptoms in schizophrenics // Pharmacopsychiatry. – 1988. – Vol. 21. – P... 389–390. 30.Rao M.L., Moler H.J. Biochemical findings of negative symptoms in schizophrenia and their putative relevance to pharma- 1. Allison D.B., Casey D.E. Antipsychotic-induced weight gain: a review of the literature // J. Clin. Psychiatry. – 2001. – Vol. 62. – P. 22–31. 2. Allison D.B., Mentore J.L., Heo M. et al. Antipsychotic induced weight gain: a comprehensive research synthesis // Am. J. Psychiatry. – 1999. – Vol. 156. – P. 1686–1696. 3. Arvanitis L.A., Miller B.G. Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: a comparison with haloperidol and placebo: the Seroquel Trial 13 Study Group // Biol. Psychiatry. – 1997. – Vol. 42. – 233–246. 4. Beasley C.M.Jr., Hamilton S.H., Crawford A.M. et al. Olanzapine versus haloperidol: acute phase results of the international double-blind trial // Eur. Neuropsychopharmacol. – 1997. – Vol. 7. – P. 125–137. 5. Beasley C.M.Jr., Sanger T., Satterlee W. et al. Olanzapine versus placebo: results of a double-blind, fixed-dose olanzapine trial // Psychopharmacology. – 1996. – Vol. 124. – P. 159–167. 6. Beasley C.M.Jr., Tollefson G., Tran P. et al. Olanzapine versus placebo and haloperidol: acute phase results of the North American double-blind olanzapine trial // Neuropsychopharmacology. – 1996. – Vol. 14. – P. 111–123. 7. Borison R.L., Arvanitis L.A., Miller B.G. ICl 204,636, an atypical antipsychotic: efficacy and safety in a multicenter, placebo-controlled trial in patients with schizophrenia: US Seroquel Study Group. JC/m // Psychopharmacol. – 1996. – Vol. 16. – P. 158–169. 8. Burris K.D., Molski T.F., Xu C. et al. Aripiprazole, a novel antipsychotic, is a high affinity partial agonist at human dopamine D2 receptors // J. Pharmacol. Exp. Ther. – 2002. – Vol. 302. – P. 381–389. 9. Daniel D.G., Saha A.R., Ingenito G. et al. Aripiprazole, a novel antipsychotic: overview of a phase II study result [abstract] // Int. J. Neuropsychopharmacol. – 2000. – Vol. 3, Suppl. 1. – P. S157. 10. Dickson R.A., Glazer W.M. Neuroleptic-induced hyperprolactinemia // Schizophr. Res. – 1999. – Vol. 35, Suppl. 1. – P. S75– S86. 11. Fleischhacker W.W., Meise U., Gunther V., Kurz M. Compliance with antipsychotic drug treatment: influence of side effects // Acta Psychiatr. Scand. – 1994. – Vol. 382. – P. 11–15. 12. Gury C., Canceil O., Iaria P. Antipsychotic drugs and cardiovascular safety: current studies of prolonged QT interval and risk of ventricular arrhythmia // Encephale. – 2000. – Vol. 26, N 6. – P. 62–72. 13. Inoue T., Domae M., Yamada K., Furukawa T. Effects of the novel antipsychotic agent 7-[4-[(2,3-dichlorophenyl)-1 -piperazinyl]butyoxy]3,4-dihydro-2 (1H)-quinolinone (OPC-14597) on prolactin release from the rat anterior pituitary gland // J. Pharmacol. Exp. Ther. – 1996. – Vol. 277. – P. 137–143. 14. Jordan S., Koprivica V., Chen R. et al. The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT1A receptor // Eur. J. Pharmacol. – 2002. – Vol. 441. – P. 137–140. 15. Kane J.M., Carson W.H., Sana A.R. et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder // J. Clin. Psychiatry. – 2002. – Vol. 63. – P. 763–771. 77 yet occupy high levels of these receptors // Mol. Psychiatry. – 1998. – Vol. 3. – P. 123–134. 34. Small J.G., Hirsch S.R., Arvanitis L.A. et al. Quetiapine in patients with schizophrenia: a high- and low-dose double-blind comparison with placebo: Seroquel Study Group // Arch. Gen. Psychiatry. – 1997. – Vol. 54. – P. 549–557. 35. Stahl S.M. Essential Psychopharmacology. – New York, NY: Cambridge University Press, 1996. 36. Tamminga C.A. Partial dopamine agonists in the treatment of psychosis // J. Neural Transm. – 2002. – Vol. 109. – P. 411–420. cologic treatment: a review // Neuropsychobiology. – 1994. – Vol. 30. – P. 160–172. 31.Richelson E. Receptor pharmacology of neuroleptics: relation to clinical effects // J. Clin. Psychiatry. – 1999. – Vol. 60, Suppl. 10. – P. 5–14. 32. Roth B.L., Sheffler D., Potkin S.G. Atypical antipsychotic drug action: unitary or multiple mechanisms for “atypicality” // Clin. Neurosci. In press. 33. Seeman P., Tallerico T. Antipsychotic drugs which elicit little or no parkinsonism bind more loosely than dopamine to brain D2 receptors, ARIPIPRAZOLE, AN ANTIPSYCHOTIC WITH A NOVEL MECHANISM OF ACTION, AND RISPERIDONE VS PLACEBO IN PATIENTS WITH SCHIZOPHRENIA AND SCHIZOAFFECTIVE DISORDER St. G. Potkin, A. R. Saha, M. J. Kujawa, W. H. Carson, M. Ali, E. Stock, J. Stringfellow, G. Ingenito, St. R. Marder placebo occurred at week 1 for PANSS total and positive scores with aripiprazole and risperidone and for PANSS negative scores with aripiprazole. There were no significant differences between aripiprazole and placebo in mean change from baseline in the extrapyramidal symptom rating scales. Mean prolactin levels decreased with aripiprazole but significantly increased 5-fold with risperidone. Mean change in QTc interval did not differ significantly from placebo with any active treatment group. Aripiprazole and risperidone groups showed a similar low incidence of clinically significant weight gain. Conclusions: Aripiprazole is effective, safe, and well tolerated for the positive and negative symptoms in schizophrenia and schizoaffective disorder. It is the first non-D2 receptor antagonist with clear antipsychotic effects and represents a novel treatment development for psychotic disorders. Background: Aripiprazole is a dopamine D2 receptor partial agonist with partial agonist activity at serotonin 5HT1A receptors and antagonist activity at 5HT2A receptors. This multicenter trial examined the efficacy, safety, and tolerability of aripiprazole in patients with acute exacerbation of schizophrenia or schizoaffective disorder. Methods: In this 4-week double-blind study, 404 patients were randomized to 20 mg/d (n=101) or 30 mg/d (n=101) of aripiprazole, placebo (n=103), or 6 mg/d of risperidone (n=99). Efficacy assessments included Positive and Negative Syndrome Scale (PANSS) scores and Clinical Global Impression scores. Safety and tolerability evaluations included extrapyramidal symptoms and effects on weight, prolactin, and corrected QT (QTc) interval. Results: Aripiprazole (20 and 30 mg/d) and risperidone (6 mg/d) were significantly better than placebo on all efficacy measures. Separation from 78