ÇÀËÀÈÍ: ÂÛÑÎÊÎÝÔÔÅÊÒÈÂÍÛÉ ÏÐÎÒÈÂÎÃÐÈÁÊÎÂÛÉ ÏÐÅÏÀÐÀÒ
advertisement

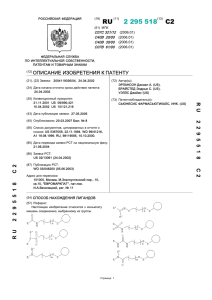
ÎÃËßÄ Èíôîðìàöèÿ êîìïàíèè ÑìèòÊëÿéí Áè÷åì Ôàðìàñüþòèêàëç Êëþ÷åâûå ñëîâà: ìèêîçû, ëå÷åíèå, ñåðòàêîíàçîë, ÇÀËÀÈÍ. ÇÀËÀÈÍ: ÂÛÑÎÊÎÝÔÔÅÊÒÈÂÍÛÉ ÏÐÎÒÈÂÎÃÐÈÁÊÎÂÛÉ ÏÐÅÏÀÐÀÒ Ðåçþìå.  îáçîðå ïðåäñòàâëåíû ðåçóëüòàòû èññëåäîâàíèé ýôôåêòèâíîñòè ïðåïàðàòà ÇÀËÀÈÍ (ñåðòàêîíàçîë) â ëå÷åíèè áîëüíûõ ñ ðàçëè÷íûìè ôîðìàìè ìèêîçîâ. Äàííûå ñâèäåòåëüñòâóþò î âûñîêîé ýôôåêòèâíîñòè ïðåïàðàòà, øèðîêîì ñïåêòðå åãî äåéñòâèÿ, íåçíà÷èòåëüíîì êîëè÷åñòâå ïîáî÷íûõ ýôôåêòîâ.  ïîñëåäíèå ãîäû îòìå÷åí ðîñò çàáîëåâàåìîñòè ìèêîçàìè. Ïî ñòàòèñòèêå îêîëî1/5 âñåãî íàñåëåíèÿ çåìíîãî øàðà ñòðàäàåò òîé èëè èíîé ôîðìîé ìèêîçîâ. Ðàçâèòèå ãðèáêîâîé èíôåêöèè îáû÷íî çàâèñèò îò êîëè÷åñòâà ãðèáêîâûõ êëåòîê, âíåäðÿþùèõñÿ â îðãàíèçì ÷åðåç ïîâðåæäåííóþ êîæó èëè ñëèçèñòûå îáîëî÷êè, è îò åãî ðåçèñòåíòíîñòè. Òÿæåñòü èíôåêöèè îáóñëîâëåíà èììóííûì îòâåòîì îðãàíèçìà íà âíåäðåíèå ïàòîãåííîãî àãåíòà. Âëèÿíèå ìíîãèõ ñåíñèáèëèçèðóþùèõ ôàêòîðîâ è íåîáîñíîâàííîå ïðèìåíåíèå àíòèñåïòè÷åñêèõ ñðåäñòâ è àíòèáèîòèêîâ, êîòîðûå èçìåíÿþò íîðìàëüíûé ñîñòàâ ìèêðîôëîðû, ïðèâåëî ê òîìó, ÷òî ïàòîãåííîñòü ãðèáîâ èçìåíèëàñü. Íàëè÷èå ìèêîçîâ, óñòîé÷èâûõ ê ëå÷åíèþ èçâåñòíûìè ïðîòèâîãðèáêîâûìè ïðåïàðàòàìè, à òàêæå ðàñïðîñòðàíåíèå ÑÏÈÄà âíåñëî îïðåäåëåííûå èçìåíåíèÿ â ïîêàçàòåëè çàáîëåâàåìîñòè ãðèáêîâûìè èíôåêöèÿìè è èõ êëèíè÷åñêèå ïðîÿâëåíèÿ. Êðîìå òîãî, íåäàâíî áûëè âûäåëåíû íåèçâåñòíûå ðàíåå âèäû ãðèáîâ, ïàòîãåííûõ äëÿ ÷åëîâåêà: Scopulariopsis brevicaulis è Trichosporon beigelii.  íàñòîÿùåå âðåìÿ âî âñåì ìèðå ïðîâîäÿòñÿ íàó÷íûå èññëåäîâàíèÿ, ïîñâÿùåííûå ðàçðàáîòêå áîëåå ýôôåêòèâíûõ è áåçîïàñíûõ ïðîòèâîãðèáêîâûõ ïðåïàðàòîâ. Èññëåäîâàòåëè Ferrer Group Research Centre (Èñïàíèÿ) ðàçðàáîòàëè âåùåñòâî, ñîäåðæàùåå 1-(2-àðèë-2-çàìåùåííóþ-ýòèë) àçîëîâóþ ãðóïïó ñ âûðàæåííûì ïðîòèâîãðèáêîâûì äåéñòâèåì è áåíçî(b)òèîôåíîâóþ ãðóïïó. Ïîñëåäíÿÿ, îêàçûâàÿ ôóíãèöèäíîå äåéñòâèå è ÿâëÿÿñü âûñîêîëèïîôèëüíûì ôðàãìåíòîì, óñèëèâàåò ìåñòíîå äåéñòâèå ýòèõ êîìïîíåíòîâ, çíà÷èòåëüíî ïîâûøàÿ èõ ïðîíèêíîâåíèå â êîæó è åå ïðèäàòêè. Íà îñíîâå ýòîãî âåùåñòâà áûë ñîçäàí ñåðòàêîíàçîë, ïðîäâèãàåìûé íà óêðàèíñêîì ðûíêå êîìïàíèåé ÑìèòÊëÿéí Áè÷åì Ôàðìàñüþòèêàëç (Âåëèêîáðèòàíèÿ) ïîä òîðãîâûì íàçâàíèåì ÇÀËÀÈÍ ïåðâûé â ìèðå ïðîòèâîãðèáêîâûé ïðåïàðàò ïðîèçâîäíîå áåíçîòèîôåíà è èìèäàçîëà, îêàçûâàþùèé êàê ôóíãèñòàòè÷åñêîå, òàê è ôóíãèöèäíîå äåéñòâèå ïðè ïðèìåíåíèè â òåðàïåâòè÷åñêèõ äîçàõ. Ñåðòàêîíàçîë îáëàäàåò øèðîêèì ñïåêòðîì äåéñòâèÿ â îòíîøåíèè âîçáóäèòåëåé, âûçûâàþùèõ èíôåêöèè êîæè è ñëèçèñòûõ îáîëî÷åê: ïàòîãåííûõ äðîææåâûõ ãðèáîâ (Candida albicans, C. tropicalis, C. pseudotropicalis, C. krusei, C. parapsilosis, C. neoformans; Torulopsis, Trichosporon è Malassezia), äåðìàòîôèòîâ (Trichophyton, Microsporum è Epidermophyton), ôèëàìåíòíûõ ãðèáîâ-îïïîðòóíèñòîâ* (Scopulariopsis, Altermania, Acremonium, Aspergillus è Fusarium), ãðàìïîëîæèòåëüíûõ (ñòàôèëîêîêêè è ñòðåïòîêîêêè, L. monocytogenes) è ãðàìîòðèöàòåëüíûõ ìèêðîîðãàíèçìîâ (E. faecium, E. faecalis, Corynebacterium spp., Bacteroides spp., P. acnes), ïðåäñòàâèòåëåé ðîäà Trichomonas. ÇÀËÀÈÍ âûñîêîàêòèâåí â îòíîøåíèè øòàììîâ C. albicans ñåðîòèïîâ A è B (ñðåäíèå çíà÷åíèÿ ìèíèìàëüíîé èíãèáèðóþùåé êîíöåíòðàöèè (ÌÈÊ): 0,21 è 0,65 ìêã/ìë ÷åðåç 24 è 48 ÷ ñîîòâåòñòâåííî), à òàêæå â îòíîøåíèè óìåðåííî ÷óâñòâèòåëüíûõ è ðåçèñòåíòíûõ ê ïðîèçâîäíûì èìèäàçîëà øòàììîâ.  òàáë. 1 ïðåäñòàâëåíà ñðàâíèòåëüíàÿ õàðàêòåðèñòèêà àêòèâíîñòè ðàçëè÷íûõ êëàññîâ ïðîòèâîãðèáêîâûõ ñðåäñòâ è ñåðòàêîíàçîëà â îòíîøåíèè âîçáóäèòåëåé, âûçûâàþùèõ èíôåêöèîííûå çàáîëåâàíèÿ êîæè è ñëèçèñòûõ îáîëî÷åê. Òàáëèöà 1 Ñïåêòð àêòèâíîñòè ðàçëè÷íûõ êëàññîâ ïðîòèâîãðèáêîâûõ ñðåäñòâ ÏðîòèâîÂîçáóäèòåëè ãðèáêîâûå Äåðìà- Äðîææå- Ïëåñíåâûå Áàêòå- Ðåçèñòåíòïðåïàðàòû òîôèòû âûå ãðèáû ãðèáû ðèè íûå ãðèáû * Ïîëèåíû ++ ++ ? Òèîêàðáàìàòû ++ ? 5-Ôòîðöèòîçèí ++ Èìèäàçîëû +++ +++ ± ± Ïèðèäîíû +++ +++ ++ ++ ? Àëëèëàìèíû +++ ? ± ± Ñåðòàêîíàçîë +++ +++ ++ +++ +++ Ìîðôîëèíû +++ +++ ? ? ± * Ãðèáû ñ ïåðåêðåñòíîé óñòîé÷èâîñòüþ ê èìèäàçîëàì è 5-ôòîðöèòîçèíó. ÇÀËÀÈÍ èìååò äâîÿêèé ìåõàíèçì äåéñòâèÿ, ÷òî îáóñëîâëåíî íàëè÷èåì â åãî ñòðóêòóðå êàê òðàäèöèîííîãî äëÿ èìèäàçîëîâ àçîëîâîãî êîëüöà, òàê è ïðèíöèïèàëüíî íîâîãî ñîåäèíåíèÿ áåíçîòèîôåíà (ðèñ. 1). * Ãðèáàìè-îïïîðòóíèñòàìè íàçûâàþòñÿ ñàïðîôèòíûå ãðèáû, êîòîðûå ïðîÿâëÿþò ïàòîãåííîñòü ïðè èììóíîêîìïðîìèññå. Ó Ê Ð À ¯ Í Ñ Ü Ê È É Ì Å Ä È × Í È É × À Ñ Î Ï È Ñ ¹ 4 (12) VII/VIII 1 9 9 9 27 ÎÃËßÄ ýôôåêòèâíîñòè ðàçëè÷íûõ ïðîòèâîãðèáêîâûõ ñðåäñòâ è ñåðòàêîíàçîëà ïðåäñòàâëåíû íà ðèñ. 4. Ðåçóëüòàòû ìíîãîöåíòðîâûõ ðàíäîìèçèðîâàííûõ èññëåäîâàíèé ïîêàçàëè, ÷òî ñåðòàêîíàçîë ïðîÿâëÿåò ìàêñèìàëüíóþ êëèíè÷åñêóþ ýôôåêòèâíîñòü: 100% ïðè äåðìàòîôèòîçàõ (Pedragosa R. et al., 1992) è îòðóáåâèäíîì (ðàçíîöâåòíîì) ëèøàå (Nassare J. et al., 1992), 95% ïðè êàíäèäîçå êîæè (Umbert P. et al., 1992). Ïî íåêîòîðûì äàííûì (Alomar C. et al., 1992), îáùàÿ êëèíè÷åñêàÿ ýôôåêòèâíîñòü ÇÀËÀÈÍÀ ñîñòàâëÿåò 98,6%. Ðèñ. 1. Ñòðóêòóðíàÿ ôîðìóëà ñåðòàêîíàçîëà Àçîëîâàÿ ñòðóêòóðà ïðåïÿòñòâóåò ñèíòåçó ýðãîñòåðèíà îäíîãî èç îñíîâíûõ êîìïîíåíòîâ ìåìáðàíû ãðèáêîâîé êëåòêè (ôóíãèñòàòè÷åñêîå äåéñòâèå), à áåíçîòèîôåí ïðîâîöèðóåò ðàçðûâ ïëàçìàòè÷åñêîé ìåìáðàíû ãðèáêîâîé êëåòêè, ÷òî ïðèâîäèò ê åå ãèáåëè (ôóíãèöèäíîå äåéñòâèå) (Agut J. et al., 1992). Áëàãîäàðÿ âûñîêîé ëèïîôèëüíîñòè áåíçîòèîôåí ãëóáîêî ïðîíèêàåò â êîæó. ×åðåç 24 ÷ 59% íàíåñåííîé äîçû ÇÀËÀÈÍÀ äîñòèãàåò ãëóáîêèõ ñëîåâ ýïèäåðìèñà (Albert C. et al., 1991), ÷åðåç 24 ÷ 72% íàíåñåííîãî ïðåïàðàòà ñîõðàíÿåò àêòèâíîñòü â ãëóáîêèõ ñëîÿõ ýïèäåðìèñà, ïðè ýòîì äåéñòâèå ïðåïàðàòà ïðîäîëæàåòñÿ â òå÷åíèå 48 ÷ (Farre M. et al., 1992). Ñåðòàêîíàçîë îáëàäàåò ïåðâè÷íîé ôóíãèöèäíîé àêòèâíîñòüþ, òî åñòü ìèíèìàëüíàÿ ôóíãèöèäíàÿ êîíöåíòðàöèÿ (ÌÔÊ) ïðèáëèæàåòñÿ ê ìèíèìàëüíîé èíãèáèðóþùåé êîíöåíòðàöèè (ÌÈÊ) (Agut J. et al., 1992) (ðèñ. 2). Ðèñ. 3. ÈÔ ðàçëè÷íûõ ïðîòèâîãðèáêîâûõ ïðåïàðàòîâ â îòíîøåíèè Candida albicans (êîíöåíòðàöèÿ 16 ìêã/ìë) Òåðàïåâòè÷åñêàÿ êîíöåíòðàöèÿ Ðèñ. 4. Êëèíè÷åñêàÿ ýôôåêòèâíîñòü ðàçëè÷íûõ ïðîòèâîãðèáêîâûõ ñðåäñòâ Ðèñ. 2. ÌÔÊ È ÌÈÊ ñåðòàêîíàçîëà ×åì ìåíüøå èíäåêñ ôóíãèöèäíîñòè (ÈÔ) (îòíîøåíèå ÌÔÊ ê ÌÈÊ), òåì âûøå ôóíãèöèäíàÿ àêòèâíîñòü ïðîòèâîãðèáêîâîãî ïðåïàðàòà. Äëÿ ñåðòàêîíàçîëà ÈÔ ïðèáëèæàåòñÿ ê åäèíèöå (ðèñ. 3). Âûñîêàÿ êëèíè÷åñêàÿ ýôôåêòèâíîñòü ÇÀËÀÈÍÀ ïîäòâåðæäåíà ðåçóëüòàòàìè ìèêîëîãè÷åñêèõ èññëåäîâàíèé (ONeill et al., 1983; Cauwenberg G.F. et al., 1984; Hay R.J. et al., 1988; Alomar A. et al., 1989). Ïîëíîå âûçäîðîâëåíèå ïîäðàçóìåâàåò êëèíè÷åñêîå èçëå÷åíèå ïðè îäíîâðåìåííîé ýðàäèêàöèè âîçáóäèòåëÿ. Ðåçóëüòàòû ñðàâíèòåëüíûõ èññëåäîâàíèé 28 ÇÀËÀÈÍ îêàçûâàåò âûðàæåííîå ôóíãèöèäíîå äåéñòâèå, ÷òî ñâîäèò ê ìèíèìóìó ðèñê ðàçâèòèÿ ðåöèäèâîâ ïîñëå ïðîâåäåííîãî êóðñà ëå÷åíèÿ (Alomar C. et al., 1992) (ðèñ. 5). Ïðèìåíåíèå ïðåïàðàòà ÇÀËÀÈÍ ïðèâîäèò ê ýðàäèêàöèè ðàçëè÷íûõ âèäîâ ãðèáîâ, â òîì ÷èñëå ðîäà Candida è Trichophyton rubrum âèäà, ÷àñòî ðåçèñòåíòíîãî ê ïðîòèâîãðèáêîâîé òåðàïèè (Raga M. et al., 1986; Multicenter double-blind trial on the efficacy and safety of sertaconazole 2% cream in comparison with miconazole 2% cream in patients suffering from cutaneous mycoses, 1989) (ðèñ. 6). Íåðåäêî ïîâåðõíîñòíûå ìèêîçû îñëîæíÿþòñÿ âòîðè÷íîé áàêòåðèàëüíîé èíôåêöèåé. Êðîìå âûðàæåííîãî ïðîòèâîãðèáêîâîãî äåéñòâèÿ ÇÀËÀÈÍ Ó Ê Ð À ¯ Í Ñ Ü Ê È É Ì Å Ä È × Í È É × À Ñ Î Ï È Ñ ¹ 4 (12) VII/VIII 1 9 9 9 ÎÃËßÄ Ðèñ. 5. ×àñòîòà ðàçâèòèÿ ðåöèäèâîâ ïðè ïðèìåíåíèè ñåðòàêîíàçîëà è ìèêîíàçîëà ÇÀËÀÈÍ îêàçûâàåò òàêæå ïðîòèâîâîñïàëèòåëüíîå äåéñòâèå.  îäíîì èç èññëåäîâàíèé, â êîòîðîì àñåïòè÷åñêîå âîñïàëåíèå èíäóöèðîâàëè êðîòîíîâûì ìàñëîì, áûëî ïðîäåìîíñòðèðîâàíî, ÷òî ïðèìåíåíèå ÇÀËÀÈÍÀ â ôîðìå êðåìà óìåíüøàåò îòåê íà 39,8% (Agut J. et al., 1996). Ëå÷åíèå ïðîòèâîãðèáêîâûìè ïðåïàðàòàìè äëÿ ìåñòíîãî ïðèìåíåíèÿ íåðåäêî ñîïðîâîæäàåòñÿ ðàçëè÷íûìè ïîáî÷íûìè ýôôåêòàìè, ñâÿçàííûìè â îñíîâíîì ñ àëëåðãè÷åñêèìè ðåàêöèÿìè è íåïåðåíîñèìîñòüþ ïðåïàðàòà.  îòíîøåíèè áåçîïàñíîñòè è ïåðåíîñèìîñòè ÇÀËÀÈÍ ïðåâîñõîäèò ëþáîé äðóãîé ïðåïàðàò äëÿ ìåñòíîãî ïðèìåíåíèÿ (ONeill et al., 1983; Cauwenberg G.F. et al., 1984; Hay R.J. et al., 1988; Multicenter double-blind trial on the efficacy and safety of sertaconazole 2% cream in comparison with miconazole 2% cream in patients suffering from cutaneous mycoses, 1989). Ðåçóëüòàòû ñðàâíèòåëüíîãî èññëåäîâàíèÿ ïîáî÷íûõ ýôôåêòîâ ðàçëè÷íûõ ïðîòèâîãðèáêîâûõ ïðåïàðàòîâ ïðåäñòàâëåíû íà ðèñ. 7. Ðèñ. 6. Ýðàäèêàöèÿ ðàçëè÷íûõ âîçáóäèòåëåé ïðè ïðèìåíåíèè ñåðòàêîíàçîëà, % îáëàäàåò àíòèáàêòåðèàëüíûì ñâîéñòâîì. Ïðåïàðàò àêòèâåí êàê â îòíîøåíèè ïåðâè÷íûõ âîçáóäèòåëåé èíôåêöèè êîæè (S. aureus, S. pyogenes), òàê è âîçáóäèòåëåé-îïïîðòóíèñòîâ (Staphylococcus epidermidis, Corynebacterium è Bacteroides), à òàêæå ïðîñòåéøèõ ðîäà Trichomonas (Prats G. et al., 1995). ÌÈÊ ðàçëè÷íûõ ïðîòèâîãðèáêîâûõ ïðåïàðàòîâ â îòíîøåíèè íåêîòîðûõ ãðàìïîëîæèòåëüíûõ è ãðàìîòðèöàòåëüíûõ ìèêðîîðãàíèçìîâ ïðåäñòàâëåíû â òàáë. 2. Òàáëèöà 2 ÌÈÊ ðàçëè÷íûõ ïðîòèâîãðèáêîâûõ ïðåïàðàòîâ Âîçáóäèòåëü ÌÈÊ, ìã/ë Áèôîíàçîë Êåòîêîíàçîë Ñåðòàêîíàçîë ÃÐÀÌÏÎËÎÆÈÒÅËÜÍÛÅ ÁÀÊÒÅÐÈÈ 416 Íå àêòèâåí 4 S. aureus 416 Íå àêòèâåí 4 S. epidermidis 416 Íå àêòèâåí 1 S. pyogenes 416 Íå àêòèâåí 4 S. agalactiae 8 L. monocytogenes ÃÐÀÌÎÒÐÈÖÀÒÅËÜÍÛÅ ÁÀÊÒÅÐÈÈ 2 E. faecium 8 E. faecalis 0,5 Corynebacterium spp. 8 Bacteroides spp. 4 P. acnes Ðèñ. 7. Ðàçâèòèå ïîáî÷íûõ ýôôåêòîâ ïðè ïðèìåíåíèè ðàçëè÷íûõ ïðîòèâîãðèáêîâûõ ïðåïàðàòîâ, % Ïðè ïðèìåíåíèè ÇÀËÀÈÍÀ íå çàðåãèñòðèðîâàíî ñëó÷àåâ êîíòàêòíîãî äåðìàòèòà (Alomar C. et al., 1992), ïðåïàðàò íå âûçûâàåò ðàçâèòèÿ ðåàêöèé ôîòîñåíñèáèëèçàöèè (Grau M.T. et al., 1992) è íå îêàçûâàåò ñèñòåìíîãî äåéñòâèÿ (Farre M. et al., 1992). Íåñìîòðÿ íà ãëóáîêîå ïðîíèêíîâåíèå ïðåïàðàòà â êîæó è åå ïðèäàòêè, à òàêæå äëèòåëüíîå ñîõðàíåíèå àêòèâíîñòè, óðîâåíü ñèñòåìíîé àáñîðáöèè ÇÀËÀÈÍÀ íàñòîëüêî íèçêèé, ÷òî ïîñëå íàðóæíîãî ïðèìåíåíèÿ ñåðòàêîíàçîë íå îïðåäåëÿåòñÿ â êðîâè ÷åëîâåêà (Farre M. et al., 1992). Ðåçóëüòàòû òîêñèêîëîãè÷åñêèõ èññëåäîâàíèé ïîêàçàëè, ÷òî ñåðòàêîíàçîë áåçîïàñåí â ñëó÷àå ïåðåäîçèðîâêè, åãî ìîæíî ïðèìåíÿòü äëèòåëüíî áåç íåãàòèâíûõ ïîñëåäñòâèé äëÿ îðãàíèçìà.  1993 ã. çà ñîçäàíèå ïðåïàðàòà ÇÀËÀÈÍ èññëåäîâàòåëÿì Ferrer Group Research Centre áûëà ïðèñóæäåíà ïðåìèÿ Ãàëåíà â îáëàñòè èññëåäîâàíèÿ è ðàçðàáîòêè ëåêàðñòâåííûõ ñðåäñòâ.  1995 ã. ÇÀËÀÈÍ áûë âêëþ÷åí â Åâðîïåéñêóþ Ôàðìàêîïåþ. Ó Ê Ð À ¯ Í Ñ Ü Ê È É Ì Å Ä È × Í È É × À Ñ Î Ï È Ñ ¹ 4 (12) VII/VIII 1 9 9 9 29 ÎÃËßÄ ËÈÒÅÐÀÒÓÐÀ Agut J. et al. (1992) Direct membrane damaging effect of Sertaconazole on Candida albicans as a mechanism of its fungicidal activity. Arzneim.-Forsch. Drug Res., 42 (5à): 721724. Agut J. et al. (1996) Centro de Investigacion Grupo Ferrer, Barcelona. Methods Findings Exp. Clin. Pharmacol., 18(4); 233234. Albert C. et al. (1991) Propiedades fisico-quimicas, determinaciones analiticas y estabilidad de nitrato de Sertaconazol. Centro de Investigacion grupo Ferrer. Barcelona. Alomar A. et al. (1989) Multicenter Phase III study to evaluate the efficacy and safety of sertaconazole 2% cream as compared to miconazole 2% cream in patients with cutaneous mycoses. XVIII Cong. Nac. Acad. Esp. Dermatol., p. 97. Alomar C. et al. (1992) Multi-centre double-blind trial on the efficacy and safety of Sertaconazole 2% cream in comparison with Miconazole 2% cream in patients suffering from cutaneous mycoses. Arzneim.-Forsch. Drug Res., 42 (5a): 767773. Cauwenberg G.F. et al. (1984) Topical ketoconazole in dermatology: A pharmacological and clinical review. Mykosen, 27(8): 395401. Farre M. et al. (1992) Pharmacokinetics and tolerance of Sertaconazole in man after repeated percutaneous administration. Arzneim.-Forsch. Drug Res., 42(5a): 752754. Grau M.T. et al. (1992) Dermal tolerance and phototoxicity studies of Sertaconazole. Arzneim.-Forsch. Drug Res., 42(5a): 746747. Hay R.J. et al. (1988) Avances en el tratamiento topico de las micosis. Springer-Verlag. Multicenter double-blind trial on the efficacy and safety of sertoconazole 2% cream in comparison with miconazole 2% cream in patients suffering from cutaneous mycoses (1989) XVIII Cong. Nac. Acad. Espan. Dermatol. (June 13, 1989, Sevilla), p. 97. Nassare J. et al. (1992) Therapeutic efficacy and safety of the new antimycotic Sertaconazole in the treatment of Pityriasis versicolor. Arzneim.-Forsch. Drug Res., 42(5a): 764767. ONeill et al. (1983) Tioconazole in the treatment of fungal infections of the skin. An International Clinical Research Program. Dermatologia, 166: 2033. Pedragosa R. et al. (1992) Therapeutic efficacy and safety of the new antimycotic Sertaconazole in the treatment of cutaneous dermatophytosis. Arzneim.-Forsch. Drug Res. Prats G. et al. (1995) Servicio de microbiologia, Hosptal de la Sta. Creu I Saint Pau, Barcelona, Rev. Esp. Quimoiterap., 8(4): 325326. ÐÅÔÅÐÀÒÈÂÍÀ Ìíîãîöåíòðîâîå äâîéíîå ñëåïîå èññëåäîâàíèå ýôôåêòèâíîñòè è áåçîïàñíîñòè ïðèìåíåíèÿ 2% êðåìà ñåðòàêîíàçîëà â ñðàâíåíèè ñ 2% êðåìîì ìèêîíàçîëà ó ïàöèåíòîâ ñ ìèêîçàìè êîæè Alomar C., Bassas S., Casas M., Crespo V., Fonseca E., et al. (1992) Multicentre double-blind triàl on efficacy and safety of sertaconazole 2% cream in comparison with miconasol 2% cream in patients suffering from cutaneous mycoses [published erratum appears in Arzneimittelforschung 1992 Jun;42(6):884]. Arzneimittelforschung, 42(5A):767-773. Ýôôåêòèâíîñòü è ïåðåíîñèìîñòü 2 % êðåìà (7õëîðî-3-[1-2,4- äèõëîðîôåíèë- 1- èë)ýòîêñèìåòèë] áåíçî[b] òèîôåíà (ñåðòàêîíàçîë, FI-7045, CAS 99592-32,2)), íàíîñèìîãî 2 ðàçà â äåíü, è 2% êðåìà ìèêîíàçîëà, íàíîñèìîãî 2 ðàçà â äåíü, èçó÷åíà ó 631 ïàöèåíòà ñ ïîâåðõíîñòíûìè ìèêîçàìè êîæè (ñåðòàêîíàçîë ó 317, ìèêîíàçîë ó 314) â äâîéíîì ñëåïîì êîíòðîëèðóåìîì ìíîãîöåíòðîâîì èññëåäîâàíèè ñ ïàðàëëåëüíûìè ãðóïïàìè. Òåðàïåâòè÷åñêóþ ýôôåêòèâíîñòü ïðåïàðàòîâ îöåíèâàëè ïî êëèíè÷åñêè îïðåäåëÿåìîìó óëó÷øåíèþ êëèíè÷åñêîãî ñîñòîÿíèÿ ïàöèåíòîâ è óìåíüøåíèþ âûðàæåííîñòè ñèìïòîìîâ, äàííûì ìèêðîñêîïè÷åñêîãî èññëå30 Raga M. et al. (1986) New imidazole antifungal agents, derived from Benzo(b)thiophene. European Journal of Medicinal Chemistry, 21(4). Umbert P. et al. (1992) Phase II study of the therapeutic efficacy and safety of the new antimycotic Sertaconazole in the treatment of superficial mycoses caused by Candida albicans. Arzneim.Forsch. Drug Res., 42(5a): 757760. ÇÀËÀ¯Í: ÂÈÑÎÊÎÅÔÅÊÒÈÂÍÈÉ ÏÐÎÒÈÃÐÈÁÊÎÂÈÉ ÏÐÅÏÀÐÀÒ Ðåçþìå.  îãëÿä³ íàâåäåí³ ðåçóëüòàòè äîñë³äæåíü ç âèâ÷åííÿ åôåêòèâíîñò³ ïðåïàðàòó ÇÀËÀ¯Í (ñåðòàêîíàçîë) ó ë³êóâàíí³ õâîðèõ ç ð³çíèìè ôîðìàìè ì³êîç³â. Äàí³ ñâ³ä÷àòü ïðî âèñîêó åôåêòèâí³ñòü ïðåïàðàòó, øèðîêèé ñïåêòð éîãî 䳿, íåçíà÷íó ê³ëüê³ñòü ïîá³÷íèõ åôåêò³â. Êëþ÷îâ³ ñëîâà: ì³êîçè, ë³êóâàííÿ, ñåðòàêîíàçîë, ÇÀËÀ¯Í. ZALAIN: HIGHLY EFFICACIOUS ANTIMYCOTIC DRUG Summary. Results of clinical trials of the drug ZALAIN (sertaconazole) in patients with various forms of cutaneous mycoses are presented in the review. Data demonstrate high efficacy of the drug, wide spectrum of its action and very few side effects. Key words: mycosis, treatment, sertaconazole, ZALAIN. Ïóáëèêàöèÿ ïîäãîòîâëåíà ïî ìàòåðèàëàì, ïðåäîñòàâëåííûì ïðåäñòàâèòåëüñòâîì êîìïàíèè ÑìèòÊëÿéí Áè÷åì Ôàðìàñüþòèêàëç â Óêðàèíå. Àäðåñ ïðåäñòàâèòåëüñòâà: Êèåâ, Êîíòðàêòîâàÿ ïë., 10À, 3-é ýòàæ Òåë.: (044) 4625947, 4906685 ²ÍÔÎÐÌÀÖ²ß äîâàíèÿ íà íàëè÷èå ãèô èëè ìèöåëèÿ â çîíå ïîðàæåíèÿ, êóëüòóðèðîâàíèÿ â öåëÿõ âûÿâëåíèÿ àêòèâíîé èíôåêöèè. Ïåðåíîñèìîñòü è áåçîïàñíîñòü îöåíèâàëè íà îñíîâàíèè äàííûõ îáùåãî àíàëèçà êðîâè, îïðîñà ïàöèåíòîâ íà ïðåäìåò íàëè÷èÿ ïîáî÷íûõ ýôôåêòîâ. Ñòåïåíü êëèíè÷åñêîãî èçëå÷åíèÿ â îáåèõ òåðàïåâòè÷åñêèõ ãðóïïàõ ïî îêîí÷àíèè ëå÷åíèÿ ñîñòàâèëà 95,6% ó ïàöèåíòîâ, ïðèìåíÿâøèõ ñåðòàêîíàçîë, è 88,1% ìèêîíàçîë, ðàçëè÷èÿ áûëè ñòàòèñòè÷åñêè äîñòîâåðíû. Ïðè ñðàâíèòåëüíîì àíàëèçå ñòàòèñòè÷åñêèõ êðèâûõ âûÿâëåíî, ÷òî ïðè ëå÷åíèè ñåðòàêîíàçîëîì ïàöèåíòû èçëå÷èâàëèñü áûñòðåå, ÷åì ïðè ëå÷åíèè ìèêîíàçîëîì, ðàçëè÷èÿ áûëè äîñòîâåðíûìè. Íåãàòèâíûå ðåçóëüòàòû ïðè ìèêðîñêîïè÷åñêîì èññëåäîâàíèè è êóëüòóðèðîâàíèè ïîäòâåðäèëè áîëåå âûñîêóþ ýôôåêòèâíîñòü ñåðòàêîíàçîëà ïî ñðàâíåíèþ ñ ìèêîíàçîëîì óæå ÷åðåç 14 äíåé ïîñëå íà÷àëà òåðàïèè. Îòðèöàòåëüíûå ðåçóëüòàòû ìèêðîáèîëîãè÷åñêèõ èññëåäîâàíèé ïîëó÷åíû ó 98,6% ïàöèåíòîâ, ïðèíèìàâøèõ ñåðòàêîíàçîë, è ó 91,7% ìèêîíàçîë; ðàçëè÷èÿ áûëè äîñòîâåðíû. Ó Ê Ð À ¯ Í Ñ Ü Ê È É Ì Å Ä È × Í È É × À Ñ Î Ï È Ñ ¹ 4 (12) VII/VIII 1 9 9 9