Отдаленные результаты лечения протоковой аденокарциномы
реклама

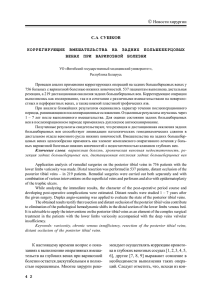
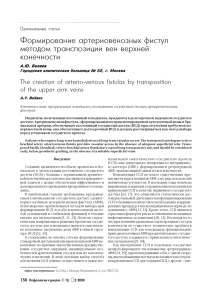
ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà, 2004, ÚÓÏ 9, ‹ 1, Ò. 129–134 ÔÓ‰ÊÂÎۉӘ̇fl ÊÂÎÂÁ‡ éÚ‰‡ÎÂÌÌ˚ ÂÁÛθڇÚ˚ ΘÂÌËfl ÔÓÚÓÍÓ‚ÓÈ ‡‰ÂÌÓ͇ˆËÌÓÏ˚ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚: Ù‡ÍÚÓ˚, ‚ÎËfl˛˘Ë ̇ ÔÓ„ÌÓÁ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl Ç. Ä. äÛ·˚¯ÍËÌ, Ä. à. ô„Ó΂, é. Ç. ŇÎÛÍÓ‚‡, Ä. Ç. äÓ˜‡ÚÍÓ‚ éÚ‰ÂÎ ‡·‰ÓÏË̇θÌÓÈ ıËÛ„ËË, è‡ÚÓÎӄӇ̇ÚÓÏ˘ÂÒÍÓ ÓÚ‰ÂÎÂÌË àÌÒÚËÚÛÚ‡ ıËÛ„ËË ËÏ. Ä.Ç. Ç˯Ì‚ÒÍÓ„Ó (‰Ë. – ‡Í‡‰. êÄåç Ç.Ñ. î‰ÓÓ‚) êÄåç ㇷӇÚÓËfl „ÛÎflˆËË ÍÎÂÚÓ˜Ì˚ı Ë ‚ËÛÒÌ˚ı ÓÌÍÓ„ÂÌÓ‚ çàà ͇̈ÂÓ„ÂÌÂÁ‡, êéçñ ËÏ. ç.ç. ÅÎÓıË̇ (‰Ë. – ˜ÎÂÌ-ÍÓ. êÄåç å.à. ч‚˚‰Ó‚) êÄåç, åÓÒÍ‚‡ çÂÒÏÓÚfl ̇ ÒÓ‚ÂÏÂÌÌ˚ ‚ÓÁÏÓÊÌÓÒÚË Î˜ÂÌËfl ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚, ÔÓ„ÌÓÁ Ú˜ÂÌËfl ˝ÚÓ„Ó Á‡·Ó΂‡ÌËfl ÓÒÚ‡ÂÚÒfl ͇ÈÌ Ì··„ÓÔËflÚÌ˚Ï. ᇠÔÓÒΉÌË 10 ÎÂÚ ‚ àÌÒÚËÚÛÚ ıËÛ„ËË ËÏ. Ä.Ç. Ç˯Ì‚ÒÍÓ„Ó êÄåç ‚˚ÔÓÎÌÂÌÓ 57 Ô‡Ì͇ÚÓ‰ÛÓ‰Â̇θÌ˚ı ÂÁÂ͈ËÈ ÔÓ ÔÓ‚Ó‰Û ÔÓÚÓÍÓ‚ÓÈ ‡‰ÂÌÓ͇ˆËÌÓÏ˚ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚. ë‰Ìflfl ÔÓÒÎÂÓÔ‡ˆËÓÌ̇fl ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË ·ÓθÌ˚ı ÒÓÒÚ‡‚Ë· 17.17 ± 1.68 ÏÂÒ., ωˇ̇ – 12 ÏÂÒ. èÓÒÎÂÓÔ‡ˆËÓÌ̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ Ô‡ˆËÂÌÚÓ‚ ÒÚ‡ÚËÒÚ˘ÂÒÍË ‰ÓÒÚÓ‚ÂÌÓ Á‡‚ËÒËÚ ÓÚ ÒÚ‡‰ËË ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡, ‡‰Ë͇θÌÓÒÚË ÓÔ‡ÚË‚ÌÓ„Ó ‚ϯ‡ÚÂθÒÚ‚‡, ÒÚÂÔÂÌË ‰ËÙÙÂÂ̈ËÓ‚ÍË ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ. ç ‚˚fl‚ÎÂÌÓ ‚ÎËflÌËfl ‚‡Ë‡ÌÚ‡ ‚˚ÔÓÎÌÂÌËfl Ô‡Ì͇ÚÓ‰ÛÓ‰Â̇θÌÓÈ ÂÁÂ͈ËË (Ò ÒÓı‡ÌÂÌËÂÏ ÊÂÎۉ͇ ËÎË ÌÂÚ) ̇ ÓÚ‰‡ÎÂÌÌ˚ ÂÁÛθڇÚ˚ ΘÂÌËfl. Ç ÓˆÂÌÍ ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl ÔÂÒÔÂÍÚË‚Ì˚Ï ÔËÁ̇ÂÚÒfl ËÁÛ˜ÂÌË ‚ ‰ËÌÓÏ ÔÓÚÓÍÓÎÂ Ò ÍÎËÌ˘ÂÒÍËÏË ‰‡ÌÌ˚ÏË Ë ·ËÓÎӄ˘ÂÒÍËı ı‡‡ÍÚÂËÒÚËÍ ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡. Long Term Survival after Pancreatic Cancer Resection: Factors of Prognosis V. A. Kubishkin, A. I. Shegolev, O. V. Balukova, A. V. Kotchatkov Department of abdominal surgery, Pathology department, A.V. Vishnevsky Institute of Surgery, RAMSei Oncogine regulation laboratory, Cancer Research Center, RAMSci, Moscow The prognosis of patients with pancreatic cancer is generally poor in spite of contemporary treatment methods. We analyzed long term results of treatment of our patients for possible prognostic factors in a retrospective trial. 57 patients (1993–2002) with histologically proven carcinoma of the head of the pancreas underwent pancreatoduodenal resection in A.V. Vishnevsky Institute of surgery, RAMSci. The mean and median survival time were 17.17 ± 1.58 and 12 months respectively. Stage of pancreatic cancer, the R0 status of the resection and histological grade had a significant influence on the survival rate. A type of the partial pancreaticoduodenectomy had no correlation with survival rate. The prognosis for these patienst is determined not only by clinicopathologic staging, but also tumor biology and molecular genetics factors. Developments in the broad field of molecular genetics may improve our ability to predict long term survival of patients with pancreatic cancer. ǂ‰ÂÌËÂ Ç êÓÒÒËË ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÂÊ„ӉÌÓ Á‡·Ó΂‡ÂÚ ÓÍÓÎÓ 13 100 ˜ÂÎÓ‚ÂÍ [1]. ÑÎfl ˝ÚËı Ô‡ˆËÂÌÚÓ‚ ÔÓ„ÌÓÁ ÊËÁÌË Ô‰ÒÚ‡‚ÎflÂÚÒfl ‰ÓÒÚ‡ÚÓ˜ÌÓ Ò¸ÂÁÌ˚Ï. ç‡ ÏÓÏÂÌÚ ÔÓÒÚ‡ÌÓ‚ÍË Ô‡‚ËθÌÓ„Ó ‰Ë‡„ÌÓÁ‡ 80–85% ·ÓθÌ˚ı ÛÊ ÌÂÓÔ‡·ÂθÌ˚ ‚ Ò‚flÁË Ò ÏÂÒÚÌ˚Ï ËÎË ÓÚ‰‡ÎÂÌÌ˚Ï ‡ÒÔÓÒÚ‡ÌÂÌËÂÏ ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡ [43]. ë‰Ìflfl ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË Ô‡ˆËÂÌÚÓ‚ Ò ÌÂÂÁÂÍÚ‡·ÂθÌ˚Ï ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÒÓÒÚ‡‚ÎflÂÚ ÓÍÓÎÓ 6–7 ÏÂÒ. [31]. èflÚËÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÔÓÒΠ‡‰Ë͇θÌÓ„Ó ÓÔ‡ÚË‚ÌÓ„Ó Î˜ÂÌËfl, ÔÓ ‰‡ÌÌ˚Ï ‡Á΢Ì˚ı ÍÎËÌËÍ, Ô‰ÒÚ‡‚ÎÂ̇ ‚ Ú‡·Î. 1. 낉ÂÌËfl Ó· ÓÚ‰‡ÎÂÌÌ˚ı ÂÁÛθڇڇı ΘÂÌËfl ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ‰Ó‚ÓθÌÓ ‡ÁÌÓ˜˂˚. êfl‰ ‡‚ÚÓÓ‚ ÔË ÓˆÂÌÍ ÂÁÛθڇÚÓ‚ ΘÂ- ÌËfl Û˜ËÚ˚‚‡˛Ú Ô‡ˆËÂÌÚÓ‚ Ò ‡Á΢Ì˚ÏË „ËÒÚÓÎӄ˘ÂÒÍËÏË ÙÓχÏË ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚, ˜ÚÓ Á‡‚˚¯‡ÂÚ ‰‡ÌÌ˚Â Ó ‚˚ÊË‚‡ÂÏÓÒÚË [34]. ÑÛ„Ë Ê ӈÂÌË‚‡˛Ú ÂÁÛθڇÚ˚ ΘÂÌËfl ÚÓθÍÓ ÔÓÚÓÍÓ‚ÓÈ ‡‰ÂÌÓ͇ˆËÌÓÏ˚ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ Í‡Í Ì‡Ë·ÓΠ˜‡ÒÚÓ ‚ÒÚ˜‡˛˘Â„ÓÒfl ÏÓÙÓÎӄ˘ÂÒÍÓ„Ó ‚‡Ë‡ÌÚ‡ ÓÔÛıÓÎÂÈ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ [5]. éÚ‰‡ÎÂÌÌ˚ ÂÁÛθڇÚ˚ ΘÂÌËfl ‚ Ú‡ÍËı ËÒÒΉӂ‡ÌËflı Á̇˜ËÚÂθÌÓ ıÛÊÂ. í‡Í, S. Nitecki Ë ÒÓ‡‚Ú. [30] ËÁ ÍÎËÌËÍË å‡ÛÓ ÔË ÍËÚ˘ÂÒÍÓÈ ÓˆÂÌÍ ÔÓÎÛ˜ÂÌÌ˚ı ÂÁÛθڇÚÓ‚ ÔÓ͇Á‡ÎË, ˜ÚÓ 5-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ÔÓÚÓÍÓ‚ÓÈ ‡‰ÂÌÓ͇ˆËÌÓÏÓÈ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ Ì 10%, Í‡Í ·˚ÎÓ ÓÔÛ·ÎËÍÓ‚‡ÌÓ ‡Ì [38], ‡ 6.8%. èÓ ‰‡ÌÌ˚Ï ç‡ˆËÓ̇θÌÓÈ ·‡Á˚ ‰‡ÌÌ˚ı ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ (National patterns of care for pancreatic cancer) ëòÄ, 5-ÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡‰ÂÌÓ͇ˆËÌÓÏÓÈ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÔÓÒΠÓÔ‡ˆËË Ì Ô‚˚¯‡ÂÚ 4% [21]. 129 9 ÔÓ‰ÊÂÎۉӘ̇fl ÊÂÎÂÁ‡ éíÑÄãÖççõÖ êÖáìãúíÄíõ ãÖóÖçàü 퇷Îˈ‡ 1. éÚ‰‡ÎÂÌÌ˚ ÂÁÛθڇÚ˚ ‡‰Ë͇θÌÓ„Ó Î˜ÂÌËfl ‡Í‡ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ Ä‚ÚÓ óËÒÎÓ Ô‡ˆËÂÌÚÓ‚ èflÚËÎÂÚÌflfl ‚˚ÊË‚‡ÂÏÓÒÚ¸, % û.à. è‡Ú˛ÚÍÓ Ë ÒÓ‡‚Ú., 2000 „. 23 0 P. Grace Ë ÒÓ‡‚Ú., 1986 „. 37 3.0 M. Connolly Ë ÒÓ‡‚Ú., 1987 „. 89 3.4 J. Lerut Ë ÒÓ‡‚Ú., 1984 „. 25 6.0 A. Cooperman, 1981 „. 70 7.0 B. Jones Ë ÒÓ‡‚Ú., 1985 „. 28 7.0 M. Sarr Ë ÒÓ‡‚Ú., 1993 „. 104 10.0 J. Klempnauer Ë ÒÓ‡‚Ú., 1996 „. 107 13.8 H. Baumel Ë ÒÓ‡‚Ú., 1994 „. 555 15.0 Y. Fong Ë ÒÓ‡‚Ú., 1995* „. 138 21.0 C. Yeo Ë ÒÓ‡‚Ú., 1999 „. 201 21.0 A. Richter Ë ÒÓ‡‚Ú., 2003** „. 122 25.4 R. Tsuchiya Ë ÒÓ‡‚Ú., 1986*** „. 103 30.3 * 臈ËÂÌÚ˚ ‚ ‚ÓÁ‡ÒÚ ‰Ó 70 ÎÂÚ; ** Ô‡ˆËÂÌÚ˚, ÍÓÚÓ˚Ï ‚˚ÔÓÎÌÂÌÓ ‚ϯ‡ÚÂθÒÚ‚Ó ‚ Ó·˙ÂÏ R0; *** Ô‡ˆËÂÌÚ˚ Ò ÓÔÛıÓθ˛ ‰Ó 2 ÒÏ. [10, 45, 51]. ÇÎËflÌË ËÌÚ‡ÓÔ‡ˆËÓÌÌÓÈ „ÂÏÓÚ‡ÌÒÙÛÁËË Í‡Í Ò‡ÏÓÒÚÓflÚÂθÌÓ„Ó Ù‡ÍÚÓ‡ ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl ÔË ‡Í ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÔËÁ̇ÂÚÒfl Ì ‚ÒÂÏË ‡‚ÚÓ‡ÏË. S. Park Ë ÒÓ‡‚Ú. [33] ÔË ‡Ì‡ÎËÁ ÓÚ‰‡ÎÂÌÌ˚ı ÂÁÛθڇÚÓ‚ ΘÂÌËfl 86 ·ÓθÌ˚ı ‡ÍÓÏ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ Ì ‚˚fl‚ËÎË ‡Á΢Ëfl ‚ ‚˚ÊË‚‡ÂÏÓÒÚË Ô‡ˆËÂÌÚÓ‚ ÌÂÁ‡‚ËÒËÏÓ ÓÚ Ôӂ‰ÂÌËfl Ò ËÌÚ‡ÓÔ‡ˆËÓÌÌÓÈ „ÂÏÓÚ‡ÌÒÙÛÁËÂÈ. çÂÁ‡‚ËÒËÏ˚Ï ÔÓ„ÌÓÒÚ˘ÂÒÍËÏ Ù‡ÍÚÓÓÏ fl‚ÎflÂÚÒfl Ë ÔÎÓˉÌÓÒÚ¸ Ñçä ÍÎÂÚÓÍ ÓÔÛıÓÎË. ÄÌÂÛÔÎÓˉÌ˚È Ì‡·Ó ıÓÏÓÒÓÏ – ˝ÚÓ ÔÎÓıÓÈ ÔÓ„ÌÓÒÚ˘ÂÒÍËÈ ÔËÁ̇Í. ë‰Ìflfl ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË Ú‡ÍËı ·ÓθÌ˚ı ‰ÓÒÚÓ‚ÂÌÓ ÏÂ̸¯Â, ˜ÂÏ ÔË ‰ËÔÎÓˉÌÓÏ Ì‡·Ó ıÓÏÓÒÓÏ [8, 39, 36]. èÓ‚ÂʉÂÌËfl „ÂÌÓ‚-ÒÛÔÔÂÒÒÓÓ‚ p53, p16INK4 ÓÔ‰ÂÎfl˛Ú ̘ۂÒÚ‚ËÚÂθÌÓÒÚ¸ ÓÔÛıÓÎË Í ıËÏËÓÚ‡ÔËË Ë ÔÎÓıÓÈ ÔÓ„ÌÓÁ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl. ïËÏËÓÚ‡Ô‚Ú˘ÂÒÍӠΘÂÌË ·ÓΠ˝ÙÙÂÍÚË‚ÌÓ Û ·ÓθÌ˚ı, ‚ ÓÔÛıÓÎflı ÍÓÚÓ˚ı Ì ‚˚fl‚ÎflÂÚÒfl ‡ÍÚË‚‡ˆËfl ÓÌÍÓ„Â̇ K-r‡s [3, 19, 28, 50]. Ç ‰‡ÌÌÓÏ ËÒÒΉӂ‡ÌËË ÔÓ‚Ó‰ËÚÒfl ÓˆÂÌ͇ ‚ÎËflÌËfl ÍÓÏÔÎÂÍÒ‡ ÔÓ„ÌÓÒÚ˘ÂÒÍËı Ù‡ÍÚÓÓ‚ ÔË ‡Í ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚, ÍÓÚÓ˚È ‚Íβ˜‡ÂÚ ÍÎËÌ˘ÂÒÍËÂ, ÏÓÙÓÎӄ˘ÂÒÍËÂ Ë ÏÓÎÂÍÛÎflÌÓ-·ËÓÎӄ˘ÂÒÍË ı‡‡ÍÚÂËÒÚËÍË ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡. å‡ÚÂË‡Î Ë ÏÂÚÓ‰ è˘ËÌÓÈ ÒÏÂÚË 97% ˝ÚËı Ô‡ˆËÂÌÚÓ‚ fl‚ÎflÂÚÒfl ˆˉ˂ ÓÒÌÓ‚ÌÓ„Ó Á‡·Ó΂‡ÌËfl [42]. ÑÛ„ËÏË ÒÎÓ‚‡ÏË, ËÁ 500 ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ‚˚ÔÓÎÌÂÌË ‡‰Ë͇θÌÓ„Ó Î˜ÂÌËfl ‚ÓÁÏÓÊÌÓ Û 100, ËÁ ÌËı 5-ÎÂÚÌËÈ Û·ÂÊ ‚ ÎÛ˜¯ÂÏ ÒÎÛ˜‡Â ÔÂÂÊË‚ÛÚ ÚÓθÍÓ ÌÂÒÍÓθÍÓ ˜ÂÎÓ‚ÂÍ. Ç ÓÔ‰ÂÎÂÌËË ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl ̇˷Óθ¯Â Á̇˜ÂÌË ËÏÂ˛Ú ÒÚ‡‰Ëfl Á‡·Ó΂‡ÌËfl (‡ÁÏ ÓÔÛıÓÎË, ÔÓ‡ÒÚ‡Ìˠ ‚ ÓÍÛʇ˛˘Ë ӄ‡Ì˚ Ë Ú͇ÌË, ‚ ÚÓÏ ˜ËÒÎÂ Ë ÔÂËÌ‚‡Î¸Ì‡fl ËÌ‚‡ÁËfl, ÎËÏÙÓ„ÂÌÌÓÂ Ë „ÂχÚÓ„ÂÌÌÓ ÏÂÚ‡ÒÚ‡ÁËÓ‚‡ÌËÂ), ÓÒÓ·ÂÌÌÓÒÚË Î˜ÂÌËfl Ô‡ˆËÂÌÚÓ‚ (‡‰Ë͇θÌÓÒÚ¸ ÓÔ‡ÚË‚ÌÓ„Ó ‚ϯ‡ÚÂθÒÚ‚‡, Ó·˙ÂÏ ÍÓ‚ÓÔÓÚÂË Ë „ÂÏÓÚ‡ÌÒÙÛÁËË, ‚ÓÁÏÓÊÌÓÒÚ¸ ‚˚ÔÓÎÌÂÌËfl Îۘ‚ÓÈ ıËÏËÓÚ‡ÔËË), ÏÓÙÓÎӄ˘ÂÒÍË ı‡‡ÍÚÂËÒÚËÍË ÓÔÛıÓÎÂÈ Ú͇ÌË („ËÒÚÓÎӄ˘ÂÒÍËÈ ‚‡Ë‡ÌÚ ÓÔÛıÓÎË, ÒÚÂÔÂ̸ ‰ËÙÙÂÂ̈ËÓ‚ÍË ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ) Ë ·ËÓÎӄ˘ÂÒÍË ÓÒÓ·ÂÌÌÓÒÚË ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡ (ÔÎÓˉÌÓÒÚ¸ Ñçä ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ, ÏÛÚ‡ˆËË ÓÔ‰ÂÎÂÌÌ˚ı „ÂÌÓ‚ Ë ‰.) [17, 26, 29, 32, 35, 42, 43, 48, 49]. êÓθ ÒÚ‡‰ËË ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡ ‚ ÓÔ‰ÂÎÂÌËË ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÌÂÓ‰ÌÓÁ̇˜ÌÓ. Ç˚fl‚ÎÂÌË Á‡·Ó΂‡ÌËfl ̇ I ÒÚ‡‰ËË ÔÓ„ÌÓÒÚ˘ÂÒÍË ·Î‡„ÓÔËflÚÌÓ, ̇ IV· – ÌÂÚ. èÓÚË‚Ó˜Ëfl ‚ ÓÔ‰ÂÎÂÌËË ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl ‚ÓÁÌË͇˛Ú ÔË II, III Ë IV‡ ÒÚ‡‰Ëflı. éÔÛ·ÎËÍÓ‚‡Ì˚ ‰‡ÌÌ˚Â, ҂ˉÂÚÂθÒÚ‚Û˛˘Ë ӷ ÓÚÒÛÚÒÚ‚ËË ÔflÏÓÈ ÍÓÂÎflˆËË ÏÂÊ‰Û ÒÚ‡‰ËÂÈ Ë ÔÓ„ÌÓÁÓÏ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl ‚ Ú‡ÍËı ÒÎÛ˜‡flı 130 ë 1993 ÔÓ 2002 „. ‚ ÓÚ‰ÂΠ‡·‰ÓÏË̇θÌÓÈ ıËÛ„ËË àÌÒÚËÚÛÚ‡ ıËÛ„ËË ËÏ. Ä.Ç. Ç˯Ì‚ÒÍÓ„Ó êÄåç ‚˚ÔÓÎÌÂÌÓ 57 Ô‡Ì͇ÚÓ‰ÛÓ‰Â̇θÌ˚ı ÂÁÂ͈ËÈ (èÑê) ·ÓθÌ˚Ï Ò ÏÓÙÓÎӄ˘ÂÒÍË ‚ÂËÙˈËÓ‚‡ÌÌÓÈ ÔÓÚÓÍÓ‚ÓÈ ‡‰ÂÌÓ͇ˆËÌÓÏÓÈ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚. ëÚ‡‰ËË ÓÔÛıÓÎÂÈ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÓÔ‰ÂÎflÎË ÔÓ Í·ÒÒËÙË͇ˆËË TNM (UICC, 1997). ë‰ÌËÈ ‚ÓÁ‡ÒÚ ·ÓθÌ˚ı 57.9 ± 1.4 „Ó‰‡, ωˇ̇ – 60 ÎÂÚ. èÓÒÎÂÓÔ‡ˆËÓÌ̇fl ÎÂڇθÌÓÒÚ¸ ÒÓÒÚ‡‚Ë· 8.7% (5 ·ÓθÌ˚ı). éÚ‰‡ÎÂÌÌ˚ ÂÁÛθڇÚ˚ ÔÓÒÎÂÊÂÌ˚ Û 52 Ô‡ˆËÂÌÚÓ‚: ÔflÏ˚Ï ÏÂÚÓ‰ÓÏ – Û 42(80.7%), ÊË‚˚ 6 (11.5%) Ô‡ˆËÂÌÚÓ‚, 1 Ô‡ˆËÂÌÚ ÛÏ ԇÍÚ˘ÂÒÍË Ò‡ÁÛ ÔÓÒΠ‚˚ÔËÒÍË ÓÚ ÒÓÔÛÚÒÚ‚Û˛˘Ëı Á‡·Ó΂‡ÌËÈ, 1 ·ÓθÌÓÈ ÛÏ ÓÚ ÓÒÚÓ„Ó ÍÓ‚ÓÚ˜ÂÌËfl ÔË ‡Á˚‚ ÒÂÎÂÁÂÌÍË ˜ÂÂÁ 5 ÏÂÒ ÔÓÒΠÓÔ‡ˆËË (̇ ‚ÒÍ˚ÚËË ÔËÁ̇ÍÓ‚ ˆˉ˂‡ ÓÒÌÓ‚ÌÓ„Ó Á‡·Ó΂‡ÌËfl Ì ‚˚fl‚ÎÂÌÓ). ëÛ‰¸·‡ 2 (3.8%) Ô‡ˆËÂÌÚÓ‚ ÔÓÒÎÂÊÂ̇ ‚ Ú˜ÂÌË 6 Ë 16 ÏÂÒ., ÔÓÒΠ˜Â„Ó Ò‚flÁ¸ Ò ÌËÏË ·˚· ÛÚÂfl̇. ëÚ‡ÚËÒÚ˘ÂÒÍËÈ ‡Ì‡ÎËÁ ‰‡ÌÌ˚ı ÔÓ‚Ó‰ËÎÒfl Ò ËÒÔÓθÁÓ‚‡ÌËÂÏ Ô‡ÍÂÚ‡ ÔÓ„‡ÏÏÌÓ„Ó Ó·ÂÒÔ˜ÂÌËfl “Statistica” (StatSoft, USA). ëÚ‡ÚËÒÚ˘ÂÒÍË ‰ÓÒÚÓ‚ÂÌÓÈ Ò˜ËÚ‡ÎË Á̇˜ÂÌË ÍÓ˝ÙÙˈËÂÌÚ‡ p < 0.05. Ç˚ÊË‚‡ÂÏÓÒÚ¸ Ô‡ˆËÂÌÚÓ‚ ÓˆÂÌË‚‡ÎË Ò ËÒÔÓθÁÓ‚‡ÌËÂÏ ÏÂÚÓ‰‡ Kaplan–Meier. êÂÁÛθڇÚ˚ Ë Ó·ÒÛʉÂÌË ë‰Ìflfl ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË ·ÓθÌ˚ı ÔÓÒΠÓÔ‡ˆËË ÒÓÒÚ‡‚Ë· 17.17 ± 1.68 ÏÂÒ, ωˇ- ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ‹1 2004 ÔÓ‰ÊÂÎۉӘ̇fl ÊÂÎÂÁ‡ äÛ·˚¯ÍËÌ Ë ‰. äÛÏÛÎflÚ˂̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ Ô‡ˆËÂÌÚÓ‚ (Cumulative Proportion Surviving) äÛÏÛÎflÚ˂̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ Ô‡ˆËÂÌÚÓ‚ (Cumulative Proportion Surviving) 1.0 1.0 0.8 0.8 0.6 0.6 0.4 0.4 0.2 0.2 0 6 12 18 24 30 36 42 48 54 60 ÇÂÏfl, ÏÂÒ T2 T3 T4 6 0 12 18 24 30 36 42 48 54 60 ÇÂÏfl, ÏÂÒ êËÒ. 1. Ç˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡ÍÓÏ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚, ÍÓÚÓ˚Ï ‚˚ÔÓÎÌÂÌÓ ‡‰Ë͇θÌÓ ÓÔ‡ÚË‚ÌӠΘÂÌË (Kaplan–Meier). êËÒ. 2. èÓÒÎÂÓÔ‡ˆËÓÌ̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ‚ Á‡‚ËÒËÏÓÒÚË ÓÚ T-ÍËÚÂËfl (Kaplan–Meier). ̇ – 12 ÏÂÒ. êËÒ. 1 ËÎβÒÚËÛÂÚ ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡ÍÓÏ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÔÓÒΠ‡‰Ë͇θÌÓÈ ÓÔ‡ˆËË. èË ‡Ì‡ÎËÁ Á‡‚ËÒËÏÓÒÚË ÔÓÒÎÂÓÔ‡ˆËÓÌÌÓÈ ‚˚ÊË‚‡ÂÏÓÒÚË Ô‡ˆËÂÌÚÓ‚ ÓÚ ÍÎËÌ˘ÂÒÍËı ı‡‡ÍÚÂËÒÚËÍ ÓÔÛıÓÎË Ë Â Ú‡ÔËË ‚˚fl‚ÎÂ̇ ‰ÓÒÚÓ‚Â̇fl Ò‚flÁ¸ ÒÓ ÒÚ‡‰ËÂÈ ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡, ‡‰Ë͇θÌÓÒÚ¸˛ Ò‡ÏÓ„Ó ÓÔ‡ÚË‚ÌÓ„Ó ‚ϯ‡ÚÂθÒÚ‚‡ Ë ÒÚÂÔÂ̸˛ ‰ËÙÙÂÂ̈ËÓ‚ÍË ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ. ç ÓÚϘÂÌÓ ‚ÎËflÌËfl ‚‡Ë‡ÌÚ‡ ‚˚ÔÓÎÌÂÌÌÓÈ èÑê (Ò ÒÓı‡ÌÂÌËÂÏ ÊÂÎۉ͇ ËÎË ÌÂÚ) ̇ ÔÓÒÎÂÓÔ‡ˆËÓÌÌÛ˛ ‚˚ÊË‚‡ÂÏÓÒÚ¸ (ÔÓ͇Á‡ÌËfl Í ‚˚ÔÓÎÌÂÌ˲ ‡Á΢Ì˚ı ‚ˉӂ èÑê ÒÏ. ‚ ÍÌË„Â Ç.Ä. äÛ·˚¯ÍË̇ Ë Ç.Ä. Ç˯Ì‚ÒÍÓ„Ó [4]). á̇˜ÂÌË ÍÓ˝ÙÙˈËÂÌÚ‡ p ‰Îfl ˝ÚËı ÍËÚÂË‚ ÓˆÂÌÍË Ô‰ÒÚ‡‚ÎÂÌ˚ ‚ Ú‡·Î. 2. èË ÓˆÂÌÍ ı‡‡ÍÚÂËÒÚËÍ Ô‚˘ÌÓÈ ÓÔÛıÓÎË, ‚ÎËfl˛˘Ëı ̇ ÔÓ„ÌÓÁ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl, ̇˷ÓΠ‚‡ÊÌ˚Ï Ô‰ÒÚ‡‚ÎflÂÚÒfl ‚ӂΘÂÌË ‚ ÓÔÛıÓ΂˚È ÔÓˆÂÒÒ ÂÚÓÔ‡Ì͇ڢÂÒÍÓÈ ÍÎÂÚ˜‡ÚÍË Ë Ï‡„ËÒڇθÌ˚ı ÒÓÒÛ‰Ó‚. ë‡ÏË ÔÓ Ò· ‡ÁÏÂ˚ ÓÔÛıÓÎË Ì Ó͇Á˚‚‡˛Ú ‰ÓÒÚÓ‚ÂÌÓ„Ó ‚ÎËflÌËfl ̇ ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË ÔÓÒΠÓÔ‡ˆËË (p = 0.494). äÛÏÛÎflÚ˂̇fl ÔÓÒÎÂÓÔ‡ˆËÓÌ̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ‚ Á‡‚ËÒËÏÓÒÚË ÓÚ T-ÍËÚÂËfl Ô‰ÒÚ‡‚ÎÂ̇ ̇ ËÒ. 2. ç‡Ë·ÓΠËÌÚÂÂÒÌÓ Ò‡‚ÌÂÌË ÓÚ‰‡ÎÂÌÌ˚ı ÂÁÛθڇÚÓ‚ ΘÂÌËfl ·ÓθÌ˚ı ‡ÍÓÏ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ̇ II Ë III ÒÚ‡‰Ëflı ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡. ùÚÓ ·ÓθÌ˚Â, Û ÍÓÚÓ˚ı ÓÔÛıÓθ ‡ÒÔÓÒÚ‡ÌflÂÚÒfl ̇ ‰‚Â̇‰ˆ‡ÚËÔÂÒÚÌÛ˛ Í˯ÍÛ, ÊÂΘÌ˚È ÔÓÚÓÍ, Ô‡‡Ô‡Ì͇ڢÂÒÍË Ú͇ÌË ÔË ÓÚÒÛÚÒÚ‚ËË ‚ӂΘÂÌËfl ÓÍÛʇ˛˘Ëı Ó„‡ÌÓ‚ Ë Ï‡„ËÒڇθÌ˚ı ÒÓÒÛ‰Ó‚ (T3N0M0 – II ÒÚ‡‰Ëfl) ËÎË ËϲÚÒfl ÎËÏÙÓ„ÂÌÌ˚ ÏÂÚ‡ÒÚ‡Á˚ (T1–3N1M0 – III ÒÚ‡‰Ëfl) ÔÓ Í·ÒÒËÙË͇ˆËË åÂʉÛ̇ӉÌÓ„Ó ÔÓÚË‚Ó‡ÍÓ‚Ó„Ó ÒÓ‚ÂÚ‡ (UICC) 1997 „. [41]. Ç ˝ÚÓÈ „ÛÔÔ ԇˆËÂÌÚÓ‚ ‰ÓÒÚÓ‚Â- Ì˚ı ‡Á΢ËÈ ‚ ‚˚ÊË‚‡ÂÏÓÒÚË Ì ÔÓÎÛ˜ÂÌÓ (p = = 0.345) (ËÒ. 3). ç‡ ÓÒÌÓ‚‡ÌËË ÓÔ‰ÂÎÂÌËfl ÚÓθÍÓ ÒÚ‡‰ËË Á‡·Ó΂‡ÌËfl Ì‚ÓÁÏÓÊÌÓ ÔÓÎÛ˜ËÚ¸ Ô‰ÒÚ‡‚ÎÂÌËÂ Ó ÚÂÏÔ‡ı ÓÒÚ‡ Ë ÔÓ„ÂÒÒËË ÓÔÛıÓÎË. í‡Í, ̇ÏË Ì ÔÓÎÛ˜ÂÌÓ ÒÚ‡ÚËÒÚ˘ÂÒÍË ‰ÓÒÚÓ‚ÂÌÓÈ ÍÓÂÎflˆËË ÏÂÊ‰Û ÒÚÂÔÂ̸˛ ‰ËÙÙÂÂ̈ËÓ‚ÍË ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ Ë ÒÚ‡‰ËÂÈ ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡ (‡ÁχÏË Ô‚˘ÌÓÈ ÓÔÛıÓÎË, ̇΢ËÂÏ ÎËÏÙÓ„ÂÌÌÓ„Ó ÏÂÚ‡ÒÚ‡ÁËÓ‚‡ÌËfl), ‡ Ú‡ÍÊ ‚ÓÁÏÓÊÌÓÒÚ¸˛ ‚˚ÔÓÎÌÂÌËfl ‡‰Ë͇θÌÓ„Ó ÓÔ‡ÚË‚ÌÓ„Ó Î˜ÂÌËfl. Ç ÚÓ Ê ‚ÂÏfl ËÏÂÂÚÒfl ‰ÓÒÚÓ‚Â̇fl Ò‚flÁ¸ ÏÂÊ‰Û ÒÚÂÔÂ̸˛ ‰ËÙÙÂÂ̈ËÓ‚ÍË ÍÎÂÚÓÍ Ë ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸˛ ÊËÁÌË ÔÓÒΠÓÔ‡ˆËË (p = 0.0006) (ËÒ. 4). èÓÎÛ˜ÂÌÌ˚ ÂÁÛθڇÚ˚ „Ó‚ÓflÚ Ó ÌÂÓ·ıÓ‰ËÏÓÒÚË ÔÓËÒ͇ Ë ËÁÛ˜ÂÌËfl ‰ÓÔÓÎÌËÚÂθÌ˚ı ı‡‡ÍÚÂËÒÚËÍ ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡ ‰Îfl ·ÓΠÚÓ˜ÌÓ„Ó ÓÔ‰ÂÎÂÌËfl ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl Û ÍÓÌÍÂÚÌÓ„Ó Ô‡ˆËÂÌÚ‡. ë ˝ÚÓÈ ˆÂθ˛ ‚Ò ·Óθ¯Â ‚ÌËχÌË ۉÂÎflÂÚÒfl ËÁÛ˜ÂÌ˲ ·ËÓÎӄ˘ÂÒÍËı, ÏÓÎÂÍÛÎflÌÓ-„ÂÌÂÚ˘ÂÒÍËı ı‡‡ÍÚÂËÒÚËÍ ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ [49, 50]. ä „Â̇Ï, ̇˷ÓΠ˜‡ÒÚÓ ‚Ó‚ÎÂ͇ÂÏ˚Ï ‚ ÔÓˆÂÒÒ Í‡ÌˆÂÓ„ÂÌÂÁ‡ ÔË ‡Í ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚, ÓÚÌÓÒflÚ ÓÌÍÓ„ÂÌ Ki-ras Ë ÓÔÛıÓ΂˚ ÒÛÔÂÒÒÓ˚ p53, p16INK4, DPC 4. èÓÚÓÓÌÍÓ„ÂÌ Ki-ras ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 퇷Îˈ‡ 2. á̇˜ÂÌË ÍÓ˝ÙÙˈËÂÌÚ‡ p ÔË ÓˆÂÌÍ ÍÓÂÎflˆËÓÌÌÓÈ Ò‚flÁË Ò ÔÓÒÎÂÓÔ‡ˆËÓÌÌÓÈ ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸˛ ÊËÁÌË äËÚÂËÈ p í 0.016 LJˇÌÚ èÑê 0.169 ꇉË͇θÌÓÒÚ¸ (R) 0.04 ëÚÂÔÂ̸ ‰ËÙÙÂÂ̈ËÓ‚ÍË (G) 0.0006 ‹1 2004 131 9* ÔÓ‰ÊÂÎۉӘ̇fl ÊÂÎÂÁ‡ éíÑÄãÖççõÖ êÖáìãúíÄíõ ãÖóÖçàü äÛÏÛÎflÚ˂̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ Ô‡ˆËÂÌÚÓ‚ (Cumulative Proportion Surviving) äÛÏÛÎflÚ˂̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ Ô‡ˆËÂÌÚÓ‚ (Cumulative Proportion Surviving) 1.0 1.0 II ÒÚ‡‰Ëfl III ÒÚ‡‰Ëfl 0.8 0.6 0.6 0.4 0.4 0.2 0.2 0 6 12 18 24 30 36 42 ÇÂÏfl, ÏÂÒ ëÚÂÔÂ̸ ‰ËÙÙÂÂ̈ËÓ‚ÍË ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ 0.8 0 ‚˚ÒÓ͇fl ÛÏÂÂÌ̇fl ÌËÁ͇fl 6 12 18 24 30 36 42 48 54 60 ÇÂÏfl, ÏÂÒ êËÒ. 3. èÓÒÎÂÓÔ‡ˆˆËÓÌ̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ‚ Á‡‚ËÒËÏÓÒÚË ÓÚ ÒÚ‡‰ËË Á‡·Ó΂‡ÌËfl (II–III ÒÚ‡‰ËË) (Kaplan-Meier). êËÒ. 4. èÓÒÎÂÓÔ‡ˆËÓÌ̇fl ‚˚ÊË‚‡ÂÏÓÒÚ¸ ·ÓθÌ˚ı ‡ÍÓÏ „ÓÎÓ‚ÍË ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ‚ Á‡‚ËÒËÏÓÒÚË ÓÚ ÒÚÂÔÂÌË ‰ËÙÙÂÂ̈ËÓ‚ÍË ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ (Kaplan-Meier). ‡ÒÔÓÎÓÊÂÌ Ì‡ ÍÓÓÚÍÓÏ ÔΘ ıÓÏÓÒÓÏ˚ 12, ‚ ÎÓÍÛÒ 13 (12p13) [23]. åÛÚ‡ˆËË ‚ ˝ÚÓÏ „ÂÌ ÔË‚Ó‰flÚ Í Â„Ó ‡ÍÚË‚‡ˆËË. ÑÎfl ÒÔÓ‡‰Ë˜ÂÒÍËı ÒÎÛ˜‡Â‚ ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ̇˷ÓΠı‡‡ÍÚÂÌ˚ ÏÛÚ‡ˆËË ‚ ÍÓ‰ÓÌ 12. ó‡ÒÚÓÚ‡ ‚˚fl‚ÎÂÌËfl ÏÛÚ‡ˆËÈ Ki-ras ‚ ÍÓ‰ÓÌ 12 ÔË ‡Í ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÍÓηÎÂÚÒfl ÓÚ 47 ‰Ó 95% [23, 40, 47]. èË ‡Í ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ÏÛÚ‡ˆËfl Ki-ras fl‚ÎflÂÚÒfl ‡ÌÌËÏ ÒÓ·˚ÚËÂÏ [15, 16, 27]. êfl‰ ‡‚ÚÓÓ‚ Ò˜ËÚ‡˛Ú, ˜ÚÓ ‡ÍÚË‚‡ˆËfl Ki-ras ‚ÓÁÏÓÊ̇ Ë ÔË „ËÔÂÔ·ÒÚ˘ÂÒÍËı ÔÓˆÂÒÒ‡ı [27]. èÓ-‚ˉËÏÓÏÛ, ÏÛÚ‡ˆËfl Ki-ras ̇·Î˛‰‡ÂÚÒfl ÚÓθÍÓ ‚ ÚÂı “‰Ó·Ó͇˜ÂÒÚ‚ÂÌÌ˚ı” ÔÓˆÂÒÒ‡ı, ‚ ÍÓÚÓ˚ı ͇ÈÌ ‚˚ÒÓÍ ÔÓÚÂ̈ˇΠÁÎÓ͇˜ÂÒÚ‚ÂÌÌÓ„Ó ÔÂÂÓʉÂÌËfl. ç‡Î˘Ë ÏÛÚ‡ˆËÈ „ÂÌÓ‚ ras ÒÍÓ ‚ÒÂ„Ó Ò‚flÁ‡ÌÓ Ò ÔÓˆÂÒÒÓÏ Ú‡ÌÒÙÓχˆËË ÍÎÂÚÓÍ Ë Ì ‚ÎËflÂÚ Ì‡ ÔÓÎËÙ‡ˆË˛ Ë ÒÔÓÒÓ·ÌÓÒÚ¸ ÍÎÂÚÓÍ Í ÏÂÚ‡ÒÚ‡ÁËÓ‚‡Ì˲ [6]. ÉÂÌ p53 ÎÓ͇ÎËÁÓ‚‡Ì ‚ ‡ÈÓÌ 17p13. îÛÌ͈ËË ·ÂÎ͇ p53 ‡ÁÌÓÓ·‡ÁÌ˚: ÍÓÌÚÓθ Á‡ ÍÎÂÚÓ˜Ì˚Ï ˆËÍÎÓÏ, ‡ÔÓÔÚÓÁÓÏ, ÂÔ‡‡ˆËÂÈ Ñçä, ÍÎÂÚÓ˜ÌÓÈ ‰ËÙÙÂÂ̈ËÓ‚ÍÓÈ, ÒÚ‡·ËθÌÓÒÚ¸˛ „ÂÌÓχ Ë ‰. [3]. íӘ˜Ì˚ ÏÛÚ‡ˆËË Ë ‰ÂΈËË ‚ „ÂÌ p53 ‰ÓÒÚ‡ÚÓ˜ÌÓ ı‡‡ÍÚÂÌ˚ ‰Îfl ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ (40–80% ̇·Î˛‰ÂÌËÈ) Ë Ì ‚˚fl‚Îfl˛ÚÒfl ÔË ıÓÌ˘ÂÒÍÓÏ Ô‡Ì͇ÚËÚ [37]. ÍÚÂÌÓ ‚˚Ô‡‰ÂÌË ӉÌÓ„Ó ÓÒÌÓ‚‡ÌËfl ‚ ˜ÂÚ‚ÂÚÓÏ ÍÓÌÒ‚‡ÚË‚ÌÓÏ ‰ÓÏÂÌ ·ÂÎ͇ (˝ÍÁÓ̇ı 5–9) [19, 40]. ÉÂÌ p16INK4 fl‚ÎflÂÚÒfl Ú‡ÍÊ ÓÔÛıÓ΂˚Ï ÒÛÔÂÒÒÓÓÏ Ë ‡ÒÔÓÎÓÊÂÌ ‚ ÎÓÍÛÒ 9p21. ùÍÒÔÂÒÒËÛÂÏ˚È ËÏ ·ÂÎÓÍ Û˜‡ÒÚ‚ÛÂÚ ‚ „ÛÎflˆËË ÍÎÂÚÓ˜ÌÓ„Ó ˆËÍ· [3]. ÉÂÌ DPC 4 (Deleted in Pancreatic Cancer) [ÒËÌÓÌËÏ Smad4] ‡ÒÔÓÎÓÊÂÌ ‚ 18q21. ÅÂÎÓÍ DPC 4 ‚˚ÔÓÎÌflÂÚ ‚‡ÊÌÛ˛ Óθ ‚ „ÛÎflˆËË Ô‰‡˜Ë Ò˄̇· ‚ β-Ú‡ÌÒÙÓÏËÛ˛˘Â„Ó Ù‡ÍÚÓ‡ ÓÒÚ‡ [15]. DPC 4 Ë̇ÍÚË‚ËÓ‚‡Ì ‚ 50–90% ̇·Î˛‰ÂÌËÈ ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚. èÓÚÂfl ÙÛÌ͈ËË „Â̇ ‚ 30% ÒÎÛ˜‡Â‚ Ò‚flÁ‡Ì‡ Ò „ÓÏÓÁË„ÓÚÌ˚ÏË ‰ÂΈËflÏË, ‚ 20% – Ò ÔÓÚÂÂÈ „ÂÚÂÓÁË„ÓÚÌÓÒÚË ‚ ÍÓÏ·Ë̇ˆËË Ò ‚ÌÛÚÂÌÌÂÈ ÏÛÚ‡- ˆËÂÈ ‚ÚÓÓ„Ó ‡ÎÎÂÎfl [23, 40]. èË “̇ÍÓÔÎÂÌËË” ‰ÓÒÚ‡ÚÓ˜ÌÓ ·Óθ¯Ó„Ó ˜ËÒ· ÏÛÚ‡ˆËÈ ‚ Íβ˜Â‚˚ı „Â̇ı, Óڂ˜‡˛˘Ëı Á‡ ÊËÁ̉ÂflÚÂθÌÓÒÚ¸, ÚÂflÂÚÒfl ÒÔÓÒÓ·ÌÓÒÚ¸ ÍÎÂÚÍË ÔÓ‰‰ÂÊË‚‡Ú¸ ÒÚ‡·ËθÌÓÒÚ¸ „ÂÌÓχ Ë Óڂ˜‡Ú¸ ‡ÔÓÔÚÓÁÓÏ (Á‡ÔÓ„‡ÏÏËÓ‚‡ÌÌÓÈ „Ë·Âθ˛) ̇ ̇ۯÂÌËfl ‚ ÌÂÏ [2]. ùÚÓ fl‚ÎflÂÚÒfl Ô‰ÔÓÒ˚ÎÍÓÈ Í ËÁÏÂÌÂÌ˲ ÔÎÓˉÌÓÒÚË Ñçä ÍÎÂÚÓÍ. ó‡ÒÚÓÚ‡ ‡ÌÂÛÔÎÓˉËÈ ‚ ÍÎÂÚ͇ı ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ Û‚Â΢˂‡ÂÚÒfl ÔÓ Ï ÓÔÛıÓ΂ÓÈ ÔÓ„ÂÒÒËË Ë ‚‡¸ËÛÂÚ ÓÚ 10 ‰Ó 79%. èË ËÒÒΉӂ‡ÌËË ÒÓ‰ÂʇÌËfl Ñçä ‚ ÍÎÂÚ͇ı ÓÔÛıÓÎË ÌÂÓÔ‡·ÂθÌ˚ı ·ÓθÌ˚ı ÔÓˆÂÌÚ ‡ÌÂÛÔÎÓˉÌ˚ı ÓÔÛıÓÎÂÈ ÒÓÒÚ‡‚ÎflÂÚ 55–75 [36, 39]. Ç Ì‡ÒÚÓfl˘Â ‚ÂÏfl ̇ÏË ÔÓ‚Ó‰ËÚÒfl ËÒÒΉӂ‡ÌË ‚ÎËflÌËfl ÏÓÎÂÍÛÎflÌÓ-„ÂÌÂÚ˘ÂÒÍËı ı‡‡ÍÚÂËÒÚËÍ, Ú‡ÍËı Í‡Í ÔÎÓˉÌÓÒÚ¸ Ñçä ÓÔÛıÓ΂˚ı ÍÎÂÚÓÍ, ÔÓÚÂfl „ÂÚÂÓÁË„ÓÚÌÓÒÚË ÎÓÍÛÒÓ‚ ‡ÒÔÓÎÓÊÂÌËfl „ÂÌÓ‚ p16INK4, DPC 4 Ë ÏÛÚ‡ˆËÈ „ÂÌÓ‚ Ki-ras (ÍÓ‰ÓÌ 12) Ë p53 (ÍÓ‰ÓÌ˚ 273, 249, 157), ̇ ÔÓÒÎÂÓÔ‡ˆËÓÌÌÛ˛ ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸ ÊËÁÌË ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚. 艂‡ËÚÂθÌ˚ ‰‡ÌÌ˚ ˝ÚÓ„Ó ËÒÒΉӂ‡ÌËfl ÔÓÁ‚ÓÎfl˛Ú ÓÚÏÂÚËÚ¸ ÌÂÍÓÚÓ˚ ÚẨÂ̈ËË. åÛÚ‡ˆËË „Â̇ Ki-ras ‚˚fl‚Îfl˛ÚÒfl ‚ 60% ̇·Î˛‰ÂÌËÈ. èÓÚÂfl „ÂÚÂÓÁË„ÓÚÌÓÒÚË „Â̇ DPC 4 ‚˚fl‚ÎflÂÚÒfl ̇ ÔÓÁ‰ÌËı ÒÚ‡‰Ëflı Ë ‡ÒÒÓˆËËÓ‚‡Ì‡ Ò Ì·Óθ¯ÓÈ ÔÓ‰ÓÎÊËÚÂθÌÓÒÚ¸˛ ÔÓÒÎÂÓÔ‡ˆËÓÌÌÓÈ ÊËÁÌË Ô‡ˆËÂÌÚÓ‚. í‡ÍËÏ Ó·‡ÁÓÏ, ÓÔ‰ÂÎÂÌË ÒÚ‡‰ËË ‡Í‡ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ ̇ ‚ÒÂı ˝Ú‡Ô‡ı Θ·ÌÓ„Ó ÔÓˆÂÒÒ‡ ÌÂÓ·ıÓ‰ËÏÓ ‰Îfl ‚˚·Ó‡ ‡‰ÂÍ‚‡ÚÌÓÈ Ú‡ÍÚËÍË ‚‰ÂÌËfl ÍÓÌÍÂÚÌÓ„Ó Ô‡ˆËÂÌÚ‡ Ë ÓÔ‰ÂÎÂÌËfl ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl Á‡·Ó΂‡ÌËfl. àÁÛ˜ÂÌË هÍÚÓÓ‚, ‚ÎËfl˛˘Ëı ̇ ÔÓ„ÌÓÁ Á‡·Ó΂‡ÌËfl, ÔÓ͇Á˚‚‡ÂÚ ÌÂÓ·ıÓ‰ËÏÓÒÚ¸ ‰ÂڇθÌÓ„Ó ËÁÛ˜ÂÌËfl ‡ÒÔÓÒÚ‡ÌÂÌÌÓÒÚË ÓÔÛıÓÎÂ‚Ó„Ó ÔÓˆÂÒÒ‡ ̇ ÂÚÓÔ‡Ì͇ڢÂÒÍÛ˛ ÍÎÂÚ˜‡ÚÍÛ Ë Ï‡„ËÒڇθÌ˚ ÒÓÒÛ‰˚, ÎËÏÙÓ„ÂÌÌÓ„Ó ÏÂÚ‡ÒÚ‡ÁËÓ‚‡ÌËfl. èÂÒÔÂÍÚË‚Ì˚ÏË ÔËÁ̇˛ÚÒfl ËÒÒΉӂ‡ÌËfl, ̇ԇ‚- 132 ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ‹1 2004 ÔÓ‰ÊÂÎۉӘ̇fl ÊÂÎÂÁ‡ äÛ·˚¯ÍËÌ Ë ‰. ÎÂÌÌ˚ Ì ÚÓθÍÓ Ì‡ ËÁÛ˜ÂÌË ÍÎËÌ˘ÂÒÍËı ‰ÂÚÂÏË̇ÌÚ ÔÓ„ÌÓÁ‡ Ú˜ÂÌËfl ·ÓÎÂÁÌË, ÌÓ Ë Ì‡ ÔÓËÒÍ ·ËÓÎӄ˘ÂÒÍËı ı‡‡ÍÚÂËÒÚËÍ, ÍÓÚÓ˚ ‰‡˛Ú Ô‰ÒÚ‡‚ÎÂÌËÂ Ó ÁÎÓ͇˜ÂÒÚ‚ÂÌÌÓÏ ÔÓÚÂ̈ˇÎ ÓÔÛıÓÎË. ëÔËÒÓÍ ÎËÚ‡ÚÛ˚ 1. ÄÍÒÂθ Ö.å., ч‚˚‰Ó‚ å.à., 쯇ÍÓ‚ í.à. áÎÓ͇˜ÂÒÚ‚ÂÌÌ˚ ÌÓ‚ÓÓ·‡ÁÓ‚‡ÌËfl ÊÂÎÛ‰Ó˜ÌÓ-Í˯˜ÌÓ„Ó Ú‡ÍÚ‡: ÓÒÌÓ‚Ì˚ ÒÚ‡ÚËÒÚ˘ÂÒÍË ÔÓ͇Á‡ÚÂÎË Ë ÚẨÂ̈ËË // ëÓ‚ÂÏÂÌ̇fl ÓÌÍÓÎÓ„Ëfl. 2001. í. 3. ‹ 4. 2. ä‡Ô˯ÂÌÍÓ Ä.à., ÄÌÚÓÌÓ‚ Ç.É., ÅËÚÂÌÍÓ Ä.Å. Ë ‰. éÌÍÓχÍÂ˚ Ë Ëı ‰Ë‡„ÌÓÒÚ˘ÂÒÍÓ Á̇˜ÂÌË // ÇÓÂÌÌÓ-ωˈËÌÒ͇fl ‡Í‡‰ÂÏËfl. ë.-èÂÚ·ۄ, 1999. 3. äÓÔÌËÌ Å.è. å˯ÂÌË ‰ÂÈÒÚ‚Ëfl ÓÌÍÓ„ÂÌÓ‚ Ë ÓÔÛıÓ΂˚ı ÒÛÔÂÒÒÓÓ‚: Íβ˜ Í ÔÓÌËχÌ˲ ·‡ÁÓ‚˚ı ÏÂı‡ÌËÁÏÓ‚ ͇̈ÂÓ„ÂÌÂÁ‡ (Ó·ÁÓ) // ÅËÓıËÏËfl. 2000. ‹ 1. 4. äÛ·˚¯ÍËÌ Ç.Ä., Ç˯Ì‚ÒÍËÈ Ç.Ä. ê‡Í ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ // å.: å‰ԇÍÚË͇. å., 2003. 5. è‡Ú˛ÚÍÓ û.à., äÓÚÂθÌËÍÓ‚ Ä.É., äÓÒ˚‚ Ç.û., åËı‡ÈÎÓ‚ å.å., ëÓÍÓÎÓ‚‡ à.ç., 뇄‡È‰‡Í à.Ç., ÄıÏÂÚÓ‚ å.ò. ëÓ‚ÂÏÂÌÌ˚ ‰‡ÌÌ˚Â Ó ‚ÓÁÏÓÊÌÓÒÚflı ıËۄ˘ÂÒÍÓ„Ó Î˜ÂÌËfl ·ÓθÌ˚ı ‡ÍÓÏ ÔÓ‰ÊÂÎÛ‰Ó˜ÌÓÈ ÊÂÎÂÁ˚ Ë Ô¡ÏÔÛÎflÌÓÈ ÁÓÌ˚ // ëÓ‚ÂÏÂÌ̇fl ÓÌÍÓÎÓ„Ëfl. 2000. í. 2. ‹ 1. 6. í‡ÚÓÒflÌ Ä.É. éÌÍÓ„ÂÌ˚ // Ç ÍÌ.: ä‡ÌˆÂÓ„ÂÌÂÁ / èÓ‰ ‰. Ñ.É. á‡Ë‰ÁÂ. å.: ç‡Û˜Ì˚È ÏË, 2000. ë. 57–74. 7. Ahmad N.A., Lewis J.D., Ginsberg G.G., Haller D.G., Morris J.B., Williams N.N., Rosato E.F., Kochman M.L. Long term survival after pancreatic resection for pancreatic adenocarcinoma // Am. J. Gastroenterol. 2001. V. 96. ‹ 9. C. 2532–2534. 8. Allison D.C., Bose K.K., Hruban R.H., Piantadosi S., Dooley W.C., Boitnott J.K., Cameron J.L. Pancreatic cancer cell DNA content Correlates with long term survival after pancreatoduodenectomy // Ann. Surg. 1991. V. 214. ‹ 6. 9. Baumel H., Huguier M., Manderscheid J.C. et al. Results of resection for cancer of the exocrine pancreas: a study from the French Association of Surgery // Br. J. Surg. 1994. 81. P. 102. 10. Birk D., Fortnagel G., Formentini A., Beger H.G. Small carcinoma of the pancreas. Factors of prognostic relevance // J. Hepatobiliary Pancreat Surg. 1998. 5. P. 450– 454. 11. Connolly M.M., Dawson P.J., Michelassi F. et al. Survival in 1001 patients with carcinoma of the pancreas // Ann. Surg. 1987. 206. P. 366. 12. Cooperman A.M. Cancer of the pancreas: a dilemma in treatment // Surg. Clin. North Am. 1981. 61. P. 107. 13. Dergman S.T., Sugan M.C., Sarkar F.H., Vaitkevicus V.K. Molecular alteration associated with improved survival in pancreatic cancer patients treated with radiation or Chemotherapy // J. Hepatobiliary Pancreat Surg. 1998. 5. P. 296–272. 14. Fong Y., Blumgart L.H., Fortner J.G. et al. Pancreatic or liver resection for malignancy is safe and effective for the elderly // Ann. Srug. 1995. 222. P. 426. ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 15. Frances C.F., McCormik, Nicholas R. Lemoine Molekular biological events in the development of pancreatic cancer // The Pancreas (chapter 97) Edited by: H.G. Begger et al. 1998. 16. Gansauge F., Gansauge S., Schmidt E., Muller J., Beger H.G. Prognostic significance of molecular alterations in human pancreatic carcinoma – an immunohistological study // Langenbeck’s Arch Surg. 1998. 383. P. 152–155. 17. Gebhardt C., Meyer W., Petter M.R., Wunsch H. Prognostic factors in the operative treatment of ductal pancreatic carcinoma // Langenbeck’s Arch. Surg. 2000. 385. P. 14–20. 18. Grace P.A., Pitt H.A., Tompkins R.K. et al. Decreased morbidity and mortality after pancreatoduodenectomy // Am. J. Surg. 1986. 151. P. 141. 19. Hruban R.H., Offerhaus G.J.A., Kern S.E., Goggins M., Wilentz R.E., Yeo C.J. Tumor-suppressor genes in pancreatic cancer // J. Hepatobiliary Pancreat Surg. 1998. 5. P. 383–391. 20. Hruban R.H., Offerhaus G.J.A., Kern S.E., Goggins M., Wilentz R.E., Yeo C.J. Tumor-suppressor genes in pancreatic cancer // J. Hepatobiliary Pancreat Surg. 1998. 5. P. 383–391. 21. Janes R.H., Niederbuber J.E., Chmiel J.S. et al. National patterns of care for pancreatic cancer: results of a survey by the Commission on Cancer // Ann. Surg. 1996. 223. P. 261. 22. Jones B.A., Janger B., Taylor B.R. et al. Periampullary tumors: which ones should be resected? // Am. J. Surg. 1985. 149. P. 46. 23. Kern S.E., Hruban R.H. Molecular Genetics of Adenocarcinoma of the Pancreas // American Cancer Society Atlas of Clinical Oncology Pancreatic Cancer John L. Cameron. 2001. 274 p. 24. Klempnauer J., Ridder G.J., Bektas H. et al. Extended resections of ductal pancreatic cancer: impact on operative risk and prognosis // Oncology. 1996. 53. P. 47. 25. Lerut J.P., Gianello P.R., Otte J.B. et al. Pancreaticoduodenal resections: surgical experience and evaluation of risk factors in 103 patients // Ann. Surg. 1984. 199. P. 432. 26. Luttges J., Reinecke-Lithge A., Mollmann B., Menke M.A.O.H., Clemens A., Klimpfinger M., Sipos B., Kloppel G. Duct changes and K-rasmutations in the disease-free pancreas:analysis of type, age relation and spatial distribution // Virchows Arch. 1999. 435. P. 461– 468. 27. Luttges J., Vogel I., Menke M., Henne-Bruns D., Kremer B., Kloppel G. The retroperitoneal resection margin and vessel involvement are important factors determining survial after pancreaticoduodenectomy for ductal adenocarcinoma of the head of the pancreas // Virchows Arch. 1998. 433. P. 237–242. 28. Mangray S., King T.C. Molecular pathobiology of pancreatic adenocarcinoma // Frontiers in Bioscience. 1998. V. 15. 3. P. 1148–1160. 29. Matsumo S., Egawa S., Shubiya K., Shimamura H., Sunamura M., Takeda K., Katoh H. et al. Pancreatic cancer: curent status of treatment and survival of 16071 patients diagnosed from 1981–1996 using the Japanese National Pancreatic Cancer Database // Int J Clin Oncol. 2000. 5. P. 153–157. ‹1 2004 133 ÔÓ‰ÊÂÎۉӘ̇fl ÊÂÎÂÁ‡ éíÑÄãÖççõÖ êÖáìãúíÄíõ ãÖóÖçàü 30. Nitecki S.S., Sarr M.G., Colby T.V. et al. Long term survival after resection for ductal adenocarcinoma of the pancreas: is it really improving? // Ann. Surg. 1995. V. 221. 59. 31. Ouchi K., Sugawara T., Ono H., Fujiva T., Kamiyama Y., Kakugawa Y., Mikuni J., Yamanami H. Palliative Operation for Cancer of the Head of the Pancreas: Significance of Pancreaticoduodenectomy and Intraoperative Radiation Therapy for Survival and Quality of Life // Worls J. Surg. 1998. 22. P. 413–417. 32. Ozaki H., Hiraoka T., Mizumoto R., Matsumoto S., Matsumoto Y., Nakayama T., Tsunoda T. et al. The prognostic significance of lymph node metastasis and intrapancreatic perineural invasion in pancreatic cancer after curative resection // Surg Today Jpn., J. Surg. 1999. 29. P. 16–22. 33. Park S.J., Kim S.W., Jang J.Y., Lee K.U., Park Y.H. Intraoperative Transfusion: Is It a Real Prognostic Factor of Periampullary Cancer following Pancreatoduodenectomy? // Worls J. Surg. 2002. 26. P. 487–492. 34. Richter A., Niedergethmann M., Sturm J.W., Lorenz D., Post S., Trede M. Long-term Results of Partial Pancreaticoduodenectomy for Ductal Adenocarcinoma of the Pancreatic Head: 25-Year Experience // Worls Journal of Surgery. 2003. 3. 27. P. 324–329. 35. Ridwelski K., Meyer F., Ebert M., Malfertheiner P., Lippert H. Prognostic Parameters Determining Surviral in Pancreatic Carcinoma and, in Particular, after Palliative Treatment // Dig Dis. 2001. 19. P. 85–92. 36. Rugge M., Sonego F., Sessa F., Leandro G. et al. Nuclear NDA Content and Pathology in Radically Treated Pancreatic Carcinoma // Cancer. 1996. 77. P. 459–466. 37. Ruggeri B.A., Huang L., Begger D., Chang H. et al. Molecular Pathology of Primary and Metastatic Ductal Pancreatic Lessions // Cancer. 1997. 79. P. 700–716. 38. Sarr M.G., Behrns K.E., Heerden J.A. Total pancreatectomy: an objective analysis of its use in pancreatic cancer // Hepatogastroentrology. 1993. 40. P. 418. 39. Schichting E. et al. Ploidy and survival in resectable pancreatic cancers // Eur. J. Surgery. 1993. 159. P. 229–233. 134 40. Sirivatanauksorn V., Sirivatanauksorn Y., Lemoine N.R. Molecular pattern of ductal pancreatic cancer // Langenbeck’s Arch. Surg. 1998. 383. P. 105–115. 41. Sobin L.H., Wittekind Ch. UICC: TNM Classification of Malignant Tumors, ed 5 // New York, Wiley, 1997. 42. Sperti C., Pasquali C., Piccoli A., Pedrazzoli S. Recurrence after Resection for Ductal Adenocarcinoma of the Pancreas // World J. Surg. 1997. 21. P. 195–200. 43. Todd K.E., Reber H.A. Prognostic Considerations in Pancreatic Cancer // Atlas of Clinical Oncology, Pancreatic Cancer. London: Bc Decker Inc. Hamilton. 2001. 44. Tsuchiya R., Noda T., Harada N. et al. Collective review of small carcinomas of the pancreas // Ann. Surg. 1986. 203. P. 77–81. 45. Tsunoda T., Eto T., Tsuchiya R. Staging of pancreatic cancer: a new japanease stage classification based on TNM factors // Chapter 100. The Pancreas, Blackwell Science, 1998. 46. Wenger F.A., Peter F., Zieren J., Steiert A., Jacobi C.A., Muller J.M. Prognosis Factors in Carcinoma of the Head of the Pancreas // Dig. Surg. 2000. 17. P. 29–35. 47. Xu Z.W., Friess H., Buchler M.W. Molecular biology of pancreatic cancer // ùÍÒÔÂËÏÂÌڇθ̇fl ÓÌÍÓÎÓ„Ëfl. 2000. 22. ë. 8–14. 48. Yeo C.J., Cameron J.L. Prognostic factors in ductal pancreatic cancer // Langenbeck’s Arch. Surg. 1998. 383. P. 129–133. 49. Yeo C.J., Cameron J.L., Lillemoe K.D., Sitzmann J.V., Hruban R.H., Goodman S.N., Dooley W.C., Coleman J., Pitt H.A. Pancreaticoduodenectomy for cancer of the head of the pancreas. 201 patients // Ann. Surg. 1995. 221. P. 721–731. 50. Yeo C.J., Cameron J.L., Sohn T.A. et al. Pancreaticoduodenectomy with or without extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma // Ann. Surg. 1999. 229. P. 613. 51. Ymamoto M. A general view of pancreatic cancer in Japan and a proposal for a more practical staging sistem // Int. J. Clin. Oncology. 1999. 4. P. 267–272. ÄççÄãõ ïàêìêÉàóÖëäéâ ÉÖèÄíéãéÉàà ÚÓÏ 9 ‹1 2004