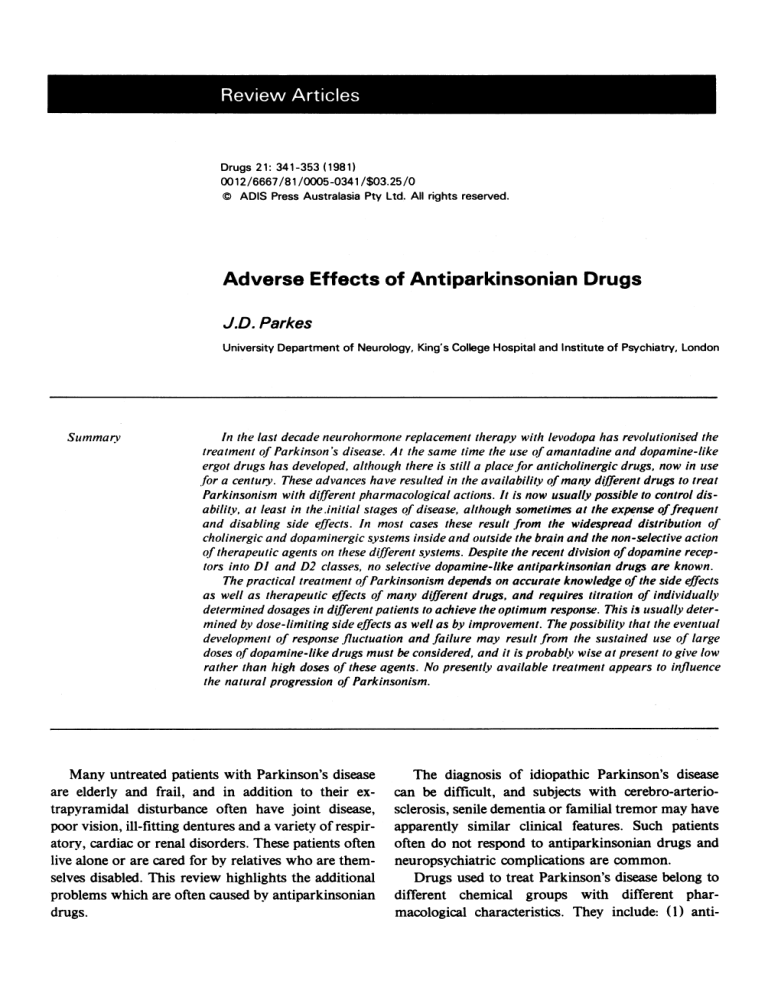
Review Articles Drugs 21: 341-353 (1981) 00 12/6667/81/0005-0341/$03.25/0 © ADIS Press Australasia Pty Ltd . All rights reserved. Adverse Effects of Antiparkinsonian Drugs J.D . Parkes University Department of Neurology, King's College Hospital and Institute of Psychiatry, London Summary In the last decade neurohormone replacement therapy with levodopa has revolutionised the treatment of Parkin son's disease. At the same time the use of amantadine and dopamine-like ergot drugs has developed, although there is still a place for anticholinergic drugs, now in use for a century. These advances have resulted in the availability of many different drugs to treat Parkinsonism with different pharmacological actions. It is now usually possible to control disability, at least in the .initial stages of disease, although sometimes at the expense offrequent and disabling side effects , In most cases these result from the widespread distribution of cholinergic and dopaminergic systems inside and outside the brain and the non-selective action of therapeutic agents on these different systems. Despite the recent division of dopamine receptors into DI and D2 classes. no selective dopamine-like antiporkinsonian drugs are known. The pract ical treatment of Parkinsonism depends on accurate knowledge of the side effects as well as therapeutic effects of many different drugs, and requires titration of individually determined dosages in different patients to achieve the optimum response . This iIJ usually deter mined by dose-limiting side effects as well as by improvement. The possibility that the eventual de velopm ent of response fluctuation and failure may result from the sustained use of large doses of dopamine-like drugs must be considered. and it is probably wise at present to give low rather than high doses of these agents. No presently available treatment appears to influence the natural progression of Parkinsonism. Many untreated patients with Parkinson's disease are elderly and frail, and in addition to their extrapyramidal disturbance often have joint disease, poor vision, ill-fitting dentures and a variety of respiratory, cardiac or renal disorders. These patients often live alone or are cared for by relatives who are themselves disabled. This review highlights the additional problems which are often caused by antiparkinsonian drugs. The diagnosis of idiopathic Parkinson 's disease can be difficult, and subjects with cerebro-arteriosclerosis, senile dementia or familial tremor may have apparently similar clinical features. Such patients often do not respond to antiparkinsonian drugs and neuropsychiatric complications are common. Drugs used to treat Parkinson 's disease belong to different chemical groups with different pharmacological characteristics. They include: (I) anti- 342 Adverse Effects of Antiparkinsonian Drugs cholinergic drugs which are thought to act centrally and reduce excess cholinergic activity in the basal ganglia; (2) levodopa which is metabolised by the enzyme dopa decarboxylase to dopamine both inside and outside the brain. Dopamine is then thought to act as a neurohormone or neurotransmitter in the basal ganglia; (3) decarboxylase inhibitors which do not penetrate the brain and have no separate antiparkinsonian effect, but combined with levodopa reduce or abolish the peripheral decarboxylation of this substance in the gut, liver and other extracerebral organs without altering the central decarboxylation of levodopa to dopamine in the brain. The commercialIy available decarboxylase inhibitors include benserazide and carbidopa, (4) amantadine, which may act by causing an increase in presynaptic dopamine release in response to nerve stimulus and also prevents presynaptic dopamine reuptake (the structure of amantadine is unrelated to that of any other antiparkinsonian drug); (5) ergot derivatives which have similar actions to dopamine, although often different side effects to levodopa, and (6) muscle relaxants, tranquillisers, central stimulants, antihistamines and the monoamine oxidase B inhibitor deprenyl. All of these drugs are effectiveto a greater or lesser extent in Parkinsonism, but adverse drug reactions are frequent. The treatment of choice in Parkinsonism is usually determined by the degree of disability. In patients with mild disability anticholinergics alone or combined with amantadine may be used. Both drugs are usually given in fixed dosages. In patients with moderate disability levodopa, usual1y combined with benserazide or carbidopa, is the most effective treatment available. Treatment must be given in individual1y determined doses and may, if necessary, be combined with anticholinergics or amantadine . In patients with severe disability, which is often accompanied by disease progression, levodopa failure and fluctuation in disability, the addition of deprenyl or bromocriptine to previous regimens occasionally produces improvement. Because of polypharmacy in the treatment of Parkinsonism, it is often difficult to attribute side effects in individual patients to one drug . An attempt should always be made to prescribe the simplest regimen that is consistent with an adequate degree of improvement. No antiparkinsonian drug should be stopped abruptly as this often results in a severe increase in disability which may last several days. Overall, antiparkinsonian drugs cause few serious biochemical problems, and adverse reactions, although frequent, are rarely life-threatening. All effective antiparkinsonian drugs may cause changes in mood or behaviour and should be avoided in patients with a history of severe neuropsychiatric disorders. Table I is a summary of the important facts that patients should know about Parkinson's disease and the possible side effectsof drug treatment. It is essential that both patients and their relatives are warned of the possibility of side effects and specifical1y of the consequences of autonomic blockade with anticholinergics, sickness and faintness with levodopa and related compounds, ankle oedema with amantadine, and uncommon but severe 'first-dose' reactions with bromocriptine. Decarboxylase inhibitors and deprenyl have not been reported to cause any serious adverse reactions. This review concentrates on the most common adverse reactions seen in clinical practice. The reported incidence of side effects of antiparkinsonian drugs varies widely and is dependent on the intensity with which they are sought and that with which patients are warned of them . Thus, figures in the text are at best approximate and refer to experience in the King's College Hospital extrapyramidal clinic. Detailed information on toxic effects and uncommon side effects of levodopa and bromocriptine has appeared in various articles in the Journal [see Drugs 2: 262 (I 97 I) ; 4: 49 (I972); 6: 364 (I 973); II: 61 (I 976); II: 329 (I 976) and 17: 365 (I 979»). J. Anticholinergic Drugs Anticholinergics are usual1y not very potent antiparkinsonian drugs although the various preparations commercially available (see table II) all reduce Adverse Effects of Antiparkinsonian Drugs 343 Table I . Summary of important facts that pat ients should know about Parkinson's disease Cause This is unknown, but Parkinson's disease is not due to any 'softening' of the brain or failure of blood flow. A few cases followed sleeping sickness in 1916 to 1926, but there have been no recent epidemics of this illness Progress In about 40% of people the severity of Parkinson's disease does not progress rapidly, and overall the condition is unlikely to shorten life Mind and senses The intellect and the senses are not affected by Parkinson's disease, at least for many years Cure As the cause is not known, there is no present cure. However, Parkinson's disease can be treated Drugs Most people will need levodopa in some form and at some stage of the illness. Levodopa is converted to the naturally occurring compound dopamine which is reduced in concentration in Parkinsonism. Levodopa will probably have to be given for life . All drugs used to treat Parkinson's disease may cause neuropsychiatric disturbance as well as other specific side effects Surgery Done previously to abolish tremor, but now largely if not entirely replaced by levodopa Diet and weight A low protein diet is possibly sometimes helpful in increasing immediate response to levodopa . Weight should be restricted Exercise May increase patient morale and reduce stiffness, but does not fundamentally alter disease tremor, rigidity and akinesia by approximately 20 % . They differ in potency, duration of action and sedative effect. All probably act centrally to prevent acetylcholine having its usual effect at receptor sites; quartenary ammonium compounds which are fully ionisedand do not penetrate the brain have little or no antiparkinsonian effect. The adverse effects of these compounds are well known and easily recognised, being mainly due to peripheral cholinergic receptor blockade. Treatment with anticholinergic drugs is usually started in fixed dosages with slow increase until an extrapyramidal effect is obvious or side effects are intolerable. Patients with postencephalitic Parkinsonism may tolerate very high dosages. Central effects of anticholinergic drugs include mild vagal and respiratory stimulation, but peripheral vagal depression usually results in a slight increase in heart rate. Changes in awareness and behaviour are of more clinical importance, Benztropine, biperiden and procyclidine all cause drowsiness, and benztropine may have a prolonged and cumulative effect. In contrast, orphenadrine occasionally causes euphoria. All centrally acting anticholinergics will cause changes in awareness, slow cerebration, inattention, restlessness, aggressive or paranoid behaviour or ideas, visual or, less commonly, tactile hallucinations or changes in mood, Intercurrent infection, concomitant administration of other drugs with anticholinergic properties such as antihistamines, butyrophenones, phenothiazines, tricyclics or other antiparkinsonian drugs, may precipitate these side effects. Mental symptoms usually recover without incident within 2 to 7 days of anticholinergic withdrawal, although physostigmine 2mg subcutaneously has been given to speed recovery (El-Yousef et al., 1972). Although phenothiazines may enhance the toxic effectsof anticholinergics, and should if possible be avoided in subjects with Parkinsonism, chlorpromazine has been used in cases of atropine poisoning (Wood and Haq, 1971). Approximately 19 to 30 % of patients with Parkinsonism given anticholinergics develop depression, confusion, delusions or hallucinations (Editorial, 1974). Toxic doses of anticholinergic drugs result in a severe mental disturbance with excitement, confusion, widely dilated pupils, flushed dry skin and fever. Increased intraocular pressure with tachycardia, pal- Adverse Effects of Antiparkinsonian Drugs Table II . Some anticholinergic drugs used in Parkinsonism Drug Benapryzine Benzhexol Benztropine Biperiden Chlorphenoxamine Cycrimine Usual daily dose (mgl 150-200 2-20 0.5-6 2-12 344 required. Neostigmine, which unlike physostigmine does not penetrate the brain or increase disability in Parkinsonism, will reverse peripheral but not central side effects of anticholinergic drugs. Eczema (Cant, 1969), retrosternal pain due to increased oesophageal reflux (Piper and Heep, 1972) and cardiac infarction (Scherf, 1973) have all been attributed to anticholinergic drugs. 150-400 5-20 Ethopropazine 40-500 Meth ixine 7.5-15 Orphenadrine 150-400 Procyclidine 7.5-30 pitations and arrhythmias, urinary retention and constipation and rapid respirations result from peripheral cholinergic blockade. Treatment is with physostigmine 1 to 2mg subcutaneously (Duvoisin and Katz, 1968), sodium thiopentone if excitement predominates and if necessary oxygen and assisted respiration. Atropine has long lasting mydriatic and cycloplegic effects. Most anticholinergics used in the treatment of Parkinsonism have less prolonged ocular effects than atropine, but difficulty in focussing is common . Dilatation of the pupil with photophobia may occur, and very rarely precipitation of angle closure glaucoma results in loss of vision (Friedman and Neumann, 1972). Reversal of anticholinergic-induced mydriasis can be achieved with thymoxamine 0.5% (Smith, 1971). Decreased salivation with anticholinergic drugs may be of value in Parkinsonism, although extreme dryness of the mouth can lead to almost total loss of teeth (Winer and Bahn, 1967). Increase in heart rate, decreased production of sweat, bronchial, lacrimal, nasal, gastric and intestinal secretions with decreased gut motility and inhibition of micturition requiring catheterisation are not uncommon. Change in diet, addition of roughage, lactulose 5 to 30ml daily, ispaghula husk 3 to 5g daily or other laxatives may be 1.1 Precautions and SpecialNotes Anticholinergics should be avoided in the presence of prostatic enlargement, pyloric stenosis or paralytic ileus, and should not be given to patients with closed angle glaucoma or a narrow angle between the iris and the cornea. Individual tolerance to anticholinergic-induced side effects differs greatly. Deaths have occurred following atropine 100mg whilst recovery has occurred after Ig. The sudden withdrawal of anticholinergics should not be attempted in patients with Parkinsonism as this may cause a considerable increase in disability. Elderly patients may require only small doses of anticholinergic drugs. Benzhexolcan be given in conventional doses to patients with impaired renal function (Bennett et al., 1973). 2. Amphetamines Amphetamines were widely used to treat patients with postencephalitic Parkinsonism in the 1930s, and often caused a considerable subjective improvement in mood or energy, but had little objective effect on extrapyramidal symptoms (Davis and Stewart, 1938). Side effects were relatively common, including dry mouth , nausea, difficulty in micturition , agitation and restlessness, insomnia and dizziness, headache, tremor and anorexia, with increasing systolic and diastolic blood pressure, tachycardia and cardiac arrhythmia in high doses. Because of the very slight therapeutic effect, frequent side effects and the possi- 345 Adverse Effects of Antiparkinsonian Drugs bility of drug misuse, leading to aggressive, antisocial or psychotic behaviour with a risk to public health, amphetamines are best avoided in the treatment of Parkinson's disease. 3. Amantadine The incidence of adverse drug reactions with amantadine 100 to 300mg daily in Parkinsonism is relatively low (Hacohen and Gurtner, 1972; table III; Rao and Pearce, 1971). Central nervous system stimulant effects which are produced by high dosages in animals occur rarely with therapeutic doses in man, and although amantadine shares pharmacological properties with amphetamine, addiction to amantadine has not been reported . Amantadine overdosage may produce an acute toxic psychosis. At very high doses (4 times the recommended dosage) convulsions have occurred (Schwab et al., 1969). Amantadine has little or no anticholinergic effect, but will potentiate neuropsychiatric disorders due to anticholinergic drugs . Disorders in awareness and hallucinations occur in 2 to 10 % of subjects treated with amantadine alone and are increasingly common with amantadine dosages higher than 200mg daily. Visual hallucinations and nocturnal confusion usually stop within a few days of amantadine withdrawal. Harper and Knothe (1973) described coloured Lilliputian hallucinations in a woman with Breughel's syndrome (orornandibular dystonia) , and a patient with cerebrovascular disease given amantadine. Symptoms of central nervous system stimulation with restlessness, nervousness and irritability occur in up to one-fifth of Parkinsonian patients treated with amantadine 100 to 300mg daily, and may account for the increase rather than decrease in tremor that occurs in some patients . Amantadine has a slight but definite alerting effect and may cause insomnia (Vitetta, 1971). Amantadine, unlike levodopa, does not usually cause dyskinesias, and the addition of amantadine to levodopa does not increase the severity of levodopa- induced involuntary movements (Godwin-Austen et aI., 1970), although Pearce (I 97 I) described a 68year-old woman who developed orofacial dyskinesias whilst taking amantadine 200mg daily. Livedo reticularis was first described in Parkinsonian patients treated with amantadine by Shealy et al. (I 970). This marbled fish net-like appearance of the skin had previously been described in collagen disorders , although not attributed to drugs . Livedo with amantadine appears to result from a pharmacological response, rather than a pathological change in blood vessels. Livedo may be more severe in cold climates than in warm surroundings and occurs to some extent in untreated normal subjects. Livedo usually resolves within 2 to 4 weeks of amantadine withdrawal. Approximately 10% of subjects treated with amantadine develop ankle oedema accompanying livedo. Oedema is usually mild in severity and first appears within 6 to 8 weeks of starting treatment. Oedema may result from changes in vascular permeability in skin blood vessels, and is usually unaccompanied by signs of heart , liver or kidney disease. It responds to diuretics but occasionally necessitates amantadine dose reduction or withdrawal. Table III . Common adverse reactions to amantadine in Parkinsonism Effect' CNS stimulation (insomnia, excitement. agitation) Approximate frequency (%) 5 to 20 Mental disturbance hallucination nocturnal confusion 15 5 Livedo up to 80 Oedema 5 to 15 1 Additionally. anorexia. dizziness. myalgia . shivering. abdominal pain and orthostatic hypotension have all been described in subjects on amantadine. Adverse Effects of Antiparkinsonian Drugs 346 Table IV. Adverse reactions to levodopa in patients with Parkinsonism Effect Approximate frequency (%)' without decarboxylase inhibitor with decarboxylase inhibitor 50 80 10 Rare Rare 90 5 40 Rare Rare Neuropsychiatric Agitation, anxiety Aggression , delusions, hallucinations, etc . Changes in mood, awareness 20 20 20 25 25 25 Involuntary movements Restlessness, chorea Dystonia 70 10 80 15 Gasrrointestinal Anore xia Nausea Abdominal pain, constipation, diarrhoea , GI bleeding Cardiovascular Postural hypotension asymptomatic symptomatic Palpitations, flushing, arrhythmia 1 15 5 Based on reports of subjects with Parkinson's disease attending the King's College Hospita l extrapyramidal disease clinic. Fahn et al. (1971) described the effects of an overdosage of amantadine (2.8g) which resulted in an acute toxic confusional state with hyperpyrexia. The patient recovered after a few days. combining it with peripherally acting dopamine decarboxylase inhibitors (vide infra). 4.1 Gastrointestinal Symptoms Vomiting, with or without nausea, occurs 20 to 90 minutes after a dose of levodopa in about 80 % of all subjects. After several months of treatment, The many adverse effects of levodopa (table IV) tolerance to the emetic effect occurs in the majority, are attributable to dopamine receptor stimulation at but not in all subjects. Nausea may sometimes be different sites inside and outside the central nervous avoided by giving low single doses of levodopa (125 system (table V). A characteristic of receptors is to 250mg), increasing daily dosage very slowly <increspecificity, but at present there is no definite clinical ments of 250 to 500mg weekly), and by always takevidence of a distinction between different types of ing levodopa with food. Although there appear to be dopamine receptors at different sites inside or outside gastric dopamine receptors, vomiting with levodopa the brain. Despite this, some progress has been made is attributable to stimulation of the medullary emetic in preventing adverse reactions to levodopa without centre, situated in the brain stem, but outside the seriously impairing the drug's therapeutic effect, by blood-brain barrier to dopamine. 4. Levodopa 347 Adverse Effects of Antiparkinsonian Drugs Gastrointestinal symptoms from levodopa may be lessened by concomitant administration of anticholinergic drugs. However, the combination of levodopa with decarboxylase inhibitors which penetrate the vomiting centre but not extrapyramidal areas of the brain, and hence prevent dopamine stimulation of medullary chernoceptors, reduces the incidence of vomiting from approximately 80 % to 15 % . To achieve adequate inhibition of peripheral decarboxylation , a minimum dose of carbidopa (75mg daily) or benserazide (I OOmg) is required. Patients taking small amounts of levodopa-decarboxylase inhibitor in fixed dose combinations may not achieve an adequate degree of inhibition of decarboxylation to prevent nausea. In addition, or alternatively, to decarboxylase inhibitors, metoclopramide 10 to 20mg, domperidone 10 to 20mg, or antacids may be given 30 to 60 minutes before levodopa. Metoclopramide 20mg penetrates the brain and will partially block the therapeutic response to levodopa, but domperidone 10 to 20mg penetrates the brain poorly if at .all and thus probably does not alter the therapeutic effects of levodopa. Despite all these measures, levodopa still occasionally may cause severe gastrointestinal disturbance. Other gastrointestinal symptoms attributable to levodopa include constipation, although this probably results from concomitant anticholinergic medication, diarrhoea, flatulence and heartburn. Gastrointestinal Table V. Distribution of dopamine-regulated systems in the body Intracerebral Nigrostriatum (motor controll Hypothalamus (growth hormone regulation) Extracerebral Pituitary (prolactin controll Autonomic ganglia limbic system (? motor con troll Pancreas Cortex (?) Spinal cord Medulla (vomiting. blood pressur e) Renal artery (renal blood flow ) bleeding has occurred in subjects with a history of peptic ulceration given levodopa. 4.2 Cardiovascular Effects Levodopa causes a fall in systolic and diastolic blood pressure because dopamine stimulates blood vessels , peripheral nerve terminals and the central nervous system (Clark et al ., 1978). Hypotension, with an average fall of systolic blood pressure of 20mm Hg occurs in the majority of subjects given levodopa, but is usually asymptomatic. However, faintness and dizziness are not uncommon at the start of treatment and may first occur in certain sensitive, disabled and hypo kinetic subjects 2 to 3 years after commencing therapy. When severe, hypotension with syncope may prevent levodopa therapy. An upright posture at night may partially reduce this side effect, and postural hypotension may be occasionally sat isfactorily controlled with elastic stockings, oral ephedrine 30 to 120mg, fludrocortisone 0.1 mg or propranolol (Duvoisin, 1970). A wide range of cardiac dysrhythmias has been described in Parkinsonian patients taking levodopa, although the incidence of transient sinus tachycardia, and atrial and ventricular extrasystoles is low and may be reduced still further by the addition of decarboxylase inhi bitors . The benefits of levodopa in practical therapy usually outweigh any risk of cardiac dysrhythmia in Parkinsonian subjects with heart disease, although such patients should be given 'Madopar' or 'Sinemet' rather than levodopa alone . Patients with Parkinson's disease are usually in an age group with a relatively high incidence of coronary artery disease, and not all dysrhythmias that appear whilst on levodopa can be necessarily attributed to the drug. 4.3 Neuropsychiatric Disorders Agitation, anxiety , elation, insom nia, drowsiness, depression, aggression, paranoid ideas, hallucina- Adverse Effects of Antiparkinsonian Drugs tions, delusions, or unmasking of dementia may occur within a few days or several years after starting levodopa, and usually present at the time of levodopa dose increase or pyrexia, or on the addition of another antiparkinsonian drug . These neuropsychiatric disorders are common with some degree of nocturnal confusion in 20 to 30 % of all Parkinsonian patients on levodopa. Improvement usually occurs 1 to 2 weeks after levodopa withdrawal , but severe psychotic symptoms may require hospitalisation. The addition of decarboxylase inhibitors to levodopa, if this permits an effective increase in levodopa dosage, will tend to increase the frequency and severity of mental disturbances. Mild psychotic symptoms, with change in mood or awareness, may be acceptable as the price of improved mobility. Levodopa-induced neuropsychiatric disorders may be treated if necessary with a psychotropic drug or non-phenothiazine derivative such as chlormethiazole. Insomnia, changes in sleep pattern or daytime narcolepsy may rarely occur in patients on levodopa (Muenter, 1970), although usually the drug has little or no effect on awareness. Elevation or depression of mood has been recorded on levodopa, although this may be a secondary effect due to alteration in severity of Parkinsonism. 348 voluntary movements. Damage to the motor system is a major determinant of levodopa dyskinesias which are unusual in subjects without motor disorders given large doses of levodopa. In some patients with Parkinson 's disease, dyskinesias first appear as treatment progresses and at dosages that have been well tolerated previously, and in other subjects dyskinesias recur at progressively lower levodopa doses. Levodopa dyskinesias vary in severity with the level of arousal and the degree of motor activation. Dyskinesias may not be troublesome to the patient and some degree of mobility accompanied by dyskinesias may be preferable to a lower degree of benefit unaccompanied by involuntary movements. However, in view of the possibility of long term levodopa response failure or response fluctuation, levodopa dosages that result in severe dyskinesias in the early years of treatment should be avoided. Indeed, the only satisfactory way to avoid levodopa dyskinesias is to reduce levodopa dosage or give small but frequent (2-hourly) oral doses oflevodopa if response fluctuation occurs with more widely separated doses. The possibility of preventing dyskinesias with the selective blockade of a 'dyskinesia-generating' population of dopamine receptors (Costall and Naylor, 1975) is of theoretical interest. Several different neuroleptic drugs will block levodopa dyskinesias to a greater or lesser extent, although usually at the expense of increased Parkinsonism (Barbeau, 1969; 4.4 Dyskinesias Bedard et al., 1978; Klawans and Weiner , 1974; Restlessness, chorea or dystonia occur in 60 to Lbermitte et al., 1977; Tarsy et al., 1975). Thus, with 90 % of all subjects with Parkinson's disease on neuroleptic treatment there is usually a reduction in otherwise optimum doses of levodopa. Dyskinesias the severity of levodopa dyskinesias as well as a are usually dose-related and of maximum severity at reduction in the therapeutic effect of levodopa. Howthe time of optimum clinical improvement from ever, with careful titration of the dosage of the neurolevodopa, although many different patterns of leptic drugs tiapride and oxiperomide, it is sometimes dyskinesia and therapeutic improvement have been possible to achieve a neuroleptic dosage that will inreported. The central origin of dyskinesias is shown hibit dyskinesias without impairment of the theraby the finding that the addition of peripherally acting peutic response (Bedard et al., 1978; Price et al., decarboxylase inhibitors to levodopa, which permits 1978). Both tiapride and oxiperomide may induce the use of large centrally effective doses of levodopa drowsiness. An alternative approach to abolish levodopa without the occurrence of nausea or vomiting, results in an increase in the frequency and severity of in- dyskinesias has been the use of low doses of 349 Adverse Effects of A ntiparkinsonian Drugs dopamine agonists rather than antagonists in an attempt to produce feedback-mediated reduction in dopamine turnover and release (Carlsson et al., 1976). However, despite the occasional report of apparently paradoxical effects of the dopamine agonists apomorphine and lergotrile in Parkinsonism (Tolosa, 1974; Weiner et al., 1978), there is insufficient evidence to conclude that low doses of dopamine-like drugs have opposite pharmacological effects to high doses in man, or that these drugs are of clinical value in the prevention of levodopa dyskinesias. 4.5 Response Fluctuation Fluctuation in disability is common in untreated Parkinsonian patients. The amplitude of Parkinsonian tremor may vary 7-fold during an hour , sudden 'freezing' episodes are common in severely disabled patients and exercise, anxiety, exhaustion, changes in arousal or motor effort all may alter the severity of akinesia. With the addition of levodopa treatment, further dose-related response swings may appear whilst involuntary levodopa dyskinesias will also interfere with voluntary movement. Response fluctuations usually increase in severity and frequency with the progression of disease and the period of levodopa treatment. Some, but not all, types of 'on-off response may be avoided by drug manipulation . Following a single oral dose of levodopa, plasma dopa reaches peak concentration after 30 minutes to 3 hours, with a mean plasma half-life of 1.08 hours without decarboxylase inhibitor and 1.6 hours with inhibitor (Dunner et al., 1971). The clinical response usually follows this time course. Attempts to delay the absorption of levodopa by administering it with food , or to increase brain penetration of levodopa by reducing dietary intake of those amino acids which compete with levodopa for transport mechanisms into the brain , may alter the duration of clinical response (Morgan et al., 1971). If despite 2-hourly administration, alone or with decarboxylase inhibitor, a steady response is not obtained, it may be necessary to consider the addition of bromocriptine or deprenyl (see below). 25 to 50 % of all Parkinsonian patients treated with levodopa for 5 years or more develop an unpredictable pattern of response or response failure. 4.6 Response Failure The disease process of Parkinson's disease is unaltered by dopamine replacement, and there is a progressive loss of dopamine receptors in the caudate nucleus which may explain the decreasing loss of response to levodopa and the shrinking period of benefit from each separate dose. It is not certain whether levodopa treatment per se may be responsible for the common appearance 2 or more years after starting treatment of response fluctuation and apparent response failure, or whether these changes are due to the unchecked progressive melanin-neurone loss in the basal ganglia. However, it is probably wise to limit levodopa early in treatment and avoid doses causing severe dyskinesias. 4.7 Other Adverse Reactions Reported urinary effects of levodopa including polyuria, incontinence, difficulty in micturition and retention may in fact result from infection, other genitourinary disease or concomitant anticholinergic drugs rather than levodopa. Patients with chronic wide angle glaucoma may be treated cautiously with levodopa, but this is contraindicated in patients with narrow angle glaucoma. The hormonal consequences of levodopa treatment (increase in growth hormone and suppression of prolactin) are usually of no clinical importance in elderly Parkinsonian subjects. Biochemical and haematological changes reported in subjects on levodopa have been reviewed in the Journal previously (Brogden et al., 1971). These changes are usually minor and include slight and usually transient rises in blood urea and nitrogen, increased serum transaminases (SGOT and SGPT>, alkaline phosphatase and bilirubin , and the occur- 350 Adverse Effects of Ant iparkinsonian Drugs renee of a positive direct Coomb's test with evidence of haemolysis. The safety of levodopa has now been demonstrated over a decade of use. No separate reactions attributable to the use of decarboxylase inhibitors have been reported in man, and their availability has made it possible to partially revise previous recommendations, precautions and contraindications to levodopa treatment. 4.8 Precautions and Special Notes Levodopa remains contraindicated in patients with severe psychoneurosis or closed angle glaucoma. It should not be given within 2 weeks of monoamine oxidase A inhibitors. Vitamin preparations which contain pyridoxine interfere with the action of levodopa, but not when this is combined with decarboxylase inhibitors. If indicated in the treatment of severe Parkinsonism, levodopa combined with a decarboxylase inhibitor can be given to patients with cardiac or renal disease, although there is a slight possibility of provoking atrial, nodal or ventricular dysrhythmias, particularly following myocardial infarction. Some caution is needed in the treatment of patients with active peptic ulcers. Periodic biochemical evaluation is unnecessary. 4.9 Drug Interactions with Levodopa Levodopa can be safely combined with other antiparkinsonian drugs and also with analgesics, tricyclic antidepressants , antidiabetic and antihypertensive drugs . Patients with Parkinsonism tolerate surgery poorly and if possible this should be done under regional or local anaesthesia. Serious adverse reactions of levodopa in combination with anaesthetics have not been reported, but if a general anaesthetic is unavoidable levodopa should be discontinued 6 hours prior to surgery . The motor effects of levodopa are diminished by phenothiazines, butyrophenones, reserpine, pyridoxine and papaverine, and enhanced by anticholinergics, amphetamine, amantadine and decarboxylase inhibitors . 5. Benserazide and Carbidopa These decarboxylase inhibitors prevent the enzymatic conversion of levodopa to dopamine . Carbidopa (l-o-methyldopa hydrazine) does not penetrate into the brain. It is usually given with levodopa in a ratio of I part carbidopa to 10 parts levodopa. The usual dose range of carbidopa is 75 to 150mg daily, given in divided doses. Benserazidewill penetrate into the brain in extremely high dosage, but at a dose of 100 to 200mg daily it causes peripheral but not central decarboxylase inhibition, The usual dose ratio of benserazide to levodopa is I to 4. No clinically obvious untoward effects have been attributed to these decarboxylase inhibitors given in these dosages with levodopa, but their use is not recommended in patients under 25 years of age or during pregnancy. 6. Ergot Derivatives Several ergot derivatives (bromocriptine, lergotrile, lisuride and pergolide)have been used in Parkinsonism, but bromocriptine is the only one of these compounds at present in widespread use. Lergotrile, but not the other compounds, has been shown to cause liver damage (Teychenne, 1979). Adverse reactions to bromocriptine and other dopamine-like ergot derivatives fall into 2 classes: first, those due to widespread and non-selective dopamine receptor stimulation; and second, those common to a number of ergot drugs , with particular reference to vascular effects (Caine et al., 1978). The dopamine stimulant actions of bromocriptine are similar in nature to those of levodopa, although the frequency of specific adverse effects with each compound is different. Tolerance to the emetic and hypotensive effect of both compounds may develop Adverse Effects of Antiparkinsonian Drugs over I to 2 months of treatment, but the therapeutic effect is undiminished . 6.1 Dopamine-like Adverse Effects of Ergot Drugs Nausea, vomiting or faintness occur in a minority of subjects (approximately 5 to 15 % ) given bromocriptine and are less troublesome than with levodopa. The incidence of these side effects depends on the care and speed with which bromocriptine is introduced: the drug should be started with a 1.25mg dose, taken with food and in bed to minimise the risk of fainting, and dose increases should not be greater than 2.5 to 5mg on alternate days. (Different patient groups allegedly show a different sensitivity to these side effects of bromocriptine , which rarely if ever causes vomiting when used to suppress postpartum lactation). If precautions are not taken a few sensitive subjects may collapse for 15 to 60 minutes after a first dose of bromocriptine, but usually recover without incident and tolerate further treatment well. Bromocriptine lowers blood pressure because it stimulates dopamine receptors on blood vessels, peripheral nerve terminals and the central nervous system. The incidence of asymptomatic hypotension with bromocriptine is comparable with that produced by levodopa in equivalent therapeutic dosages. Severe symptomatic hypotension is uncommon . 22 of over 10,000 subjects given bromocriptine have had hypotension and collapse, mainly on starting treatment, with less severe symptoms in 1.8 % of subjects with both endocrine and motor disorders (data on file, Sandoz Pharmaceuticals). Factors affecting the liability to develop serious hypotension with bromocriptine have not been definitely identified, although previous tendency to faint, presence of peripheral vascular disease, vasodilator drugs and high altitudes may all be risk factors (Parkes, 1980). Neuropsychiatric symptoms with bromocriptine are similar to those caused by levodopa alone, although with bromocriptine they may be more severe, more frequent and of longer duration, lasting 351 2 to 6 weeks after drug withdrawal. These symptoms are more common in elderly frail subjects with Parkinson's disease than in young subjects given bromocriptine to reduce hyperprolactinaemia or treat acromegaly (drug dosages in the different groups are not usually comparable). Bromocriptine causes an increased incidence of uterine tumours in rats, but apparently not in human beings. At present it may be wise to recommend that all women on bromocriptine have an annual gynaecological examination (Besser et al., 1977), although this will probably eventually prove unnecessary. Women with Parkinsonism are seldom of childbearing age: although it is recommended that bromocriptine should not be given to pregnant women , the incidenceof abortion and fetal malformation is similar in subjects who have taken bromocriptine throughout pregnancy and in the general population (Griffith et al., 1978). 6.2 Other Adverse Effects of Ergot Drugs Vascular toxicity with bromocriptine appears to be less common than with some other ergot derivatives; Raynaud's phenomenon, erythromelalgia and Livedo reticularis sometimes occur in parkinsonian patients given bromocriptine , but serious vascular or endothelial damage is very rare. 7. Deprenyl Retarding the breakdown of dopamine should prolong the antiparkinsonian effect of separate doses of levodopa and reduce symptom fluctuations when this results from rapid changes in brain dopamine levels. This can be achieved by monoamine oxidase (MAO) inhibitors, but the combination of levodopa with most available MAO inhibitors is liable to cause hypertensive crises as well as requiring rigid dietary restrictions . 2 types of MAO inhibitors are now recognised, and I-deprenyl selectively inhibits MAO type B, the predominant type in the human brain Adverse Effects of Antiparkinson ian Drugs (Glover et al., 1977). The addition of deprenyl IOmg daily to levodopa appears to enhance and prolong the antiparkinsonian effect of levodopa (Birkmayer et al., 1977; Lees et al., 1977). Although I-deprenyl is converted to I-amphetamine in the brain , and possibly the liver, the drug appears to have little or no amphetamine-like properties or side effects, and addiction or tolerance to I-deprenyl has not yet been reported . Despite the absence of side effects, if 1deprenyl does achieve a permanent place in the management of Parkinsonism, the minimal dose causing central MAO inhibition should be used. This dosage has not been defined, but may be as low as 2 to 5mg daily. References Barbeau . A.: L-dopa therap y in Park inson 's disease: a critical review of nine years' experience. Jou rnal of the Canadia n Medical Association 101: 59-68 (1969 ). Bedard . P; Parkes. J.D. and Marsden . C. D.: Effect of new dopamine-block ing agent (oxiperom ide) on drug -induced dyskinesias in Parkinson's disease and spontaneous dyskinesias, British Medical Journal I: 954-956 (197 8). Bennett. W .M.; Singer. I. and Coggins. C.H .: Gu ide to drug usage in adult patients with impaired renal function . Journal of the American Medical Association 223: 991-997 (1973 ). Besser. G .M.; Thorner. M.O.; Wass. J.A.H. ; Doniach. I.; Cant i, G .; Curling. M.; Grudziniskas, J.G . and Setchell, M.E.: Absence of uterine neoplasms in patients on bromocriptine. British Medical Journal 2: 868 (1977 ). Birkmayer, W .; Riederer, P.; Ambrozi , L. and Youdirn, M.B.H.: Implications of combined treatment with Madopar and Ideprenil in Parkinson's disease. Lancet I : 439-443 (1977) . Caine . D.B.; Williams, C .; Neoph ytides, A.; Plotkin . C, Nutt , J.G. and Teychenne , P.F.: Long-term treatment of parkinsonism with bromocriptine. Lancet I: 735-73 8 (197 8). Cant . J.S.: Iatrogen ic eye disease. Practitioner 202: 787-795 (1969). Carlsson. A.; Kehr, W. and Lindqvist, M.: The role of intraneuron al amine levels in the feedback control of dopamine. noradrenaline and 5-hydroxy-tryptamine synthesis in rat brain. Journal of Neural Tran sm ission 39: 1-19 (1976 ). Brogden . R.N.; Speight. T.M . and Avery, G.S .: Levodopa, A review of its pharmacological propert ies and therapeu tic uses with particular reference to park insonism. Drugs 2: 262-400 (197)). 352 Clark . BJ.; Scholtysik, G. and Fluckiger , E.: Cardio vascular actions of bromocriptine. Acta Endocrinologia (Suppl.) 216 : 78-81 (1978). Costall, B. and Naylor. RJ .: Neuroleptic antagoni sm of dyskinetic phenomena. European Journal of Pharmacology 33: 30 1-312 (1975 ). Davis, P.L. and Stewart . W.B.: The use of benzedrine sulfate in post-encephal itic parkinson ism. Journal of the American Medical Association 110: 1890-1892 (1938) . Dunner. D.L.; Brodie. H.K.H. and Goodwin, F.K.: Plasma DOPA response to levodopa administration in man : Effects of a peripheral decarboxylase inhibitor . Clinical Pharmacology and Therapeutic s 12: 212-217 (197)). Duvoisin , R.C.: Hypotension caused by levodopa . British Medical Journal 3: 47 (1970). Duvoisin , R.C. and Katz. R.: Reversal of central ant icholinergic syndrome in man by physostigmine. Journal of the American Medical Association 206: 1963-1965 (1968) . Editorial. Mental changes in Parkinsonism. British Medical Journal 2: 1-2 (1974). EI·Yousef, M.K.; Janowsk y, D.S.; David. J.M. and Sekerk e, HJ . Reversal of benztrop ine toxicity by physostigmine . Journ al of the Amer ican Medical Association 220 : 125 (1972) . Fahn , S.; Cradd ock. G. and Kumin, G.: Acute toxic psychosis from suicidal overdosage of amantadine. Archives of Neurology 25: 45-48 (1971). Friedman. Z. and Neumann. E.: Benzhexol-induced blindn ess in Parkinson's disease. British Medical Journal I : 60 5 () 972 ). Glover . V.; Sandler. M.; Owen. F. and Riley. GJ .: Dopamine is a monoamin e oxidase B substrate in man . Nature 265 : 80-8 1 (1977). Godwin-Austen , R.B.; Frears, c.c.; Bergmann . S.; Parkes. J .D. and Knill-Jones, R.P.: Comb ined treatment of par kinsonism with l-dopa and amantadine. Lancet 2: 383-385 (970). Griffith, R.W .; Turk alj, I. and Braun . P.: Outcome of pregnancy in mothers given bromocriptine. British Journal of Clinical Pharmacology 5: 227-231 (1978). Hacohen, H. and Gurtner. B.: Klinische pru fung des therapieseffektes von Amantadin -HCI bei morbu s parkin son. Schweizerische Medizinische Wochenschrift 102: 583-58 6 (972). Harper . R.W . and Knothe, B.: Coloured Lilliputian hallucination s with amantadine . Medical Journal of Australia I: 444-445 (1973) . Klawans, H.L. and Weiner, WJ .: Attemp ted use of haloperidol in the treatment of I-dopa induced dyskinesias. Journ al of Neurology, Neurosurgery and PSYChiatr y 37: 427-4 30 (1974). Lees. AJ .; Shaw . K.M.; Kohout, L.J.; Stern . G .M.; Elsworth . J.D.; Sandler . M. and Youdim , M.B.H.: Depren yl in Park inson's disease. Lancet 2: 791 -796 (1977) . Lherm itte, F.; Agid, Y.; Signoret, J. L. and Studler , J-M.: Les dyskinesies de 'debut et fin de dose' provoquees par la I-dopa. Revue Neuro logique 133: 297-308 (1977>. Adverse Effects of Antiparkinsonian Drugs Morgan, J.P .; Bianchine, J .R .; Spiegel, H.E .; Rivera -Calimlim, L. and Hersey, R.M.: Metabolism of levodopa in patients with Parkinson's disease. Radioactive and fluorometric assays . Archives of Neurology 25: 39-44 (1971). Muenter, M.D.: Double-blind, placebo controlled study of levodopa therapy in Parkinson's disease . Neurology 20 (Suppl .). 673 <1970>. Parkes , J .D .: Side effects of bromocriptine. New England Journal of Medicine 302 : 749 -750 (1980). Pearce, J .: Mechani sm of action of amantadine. British Medical Journal 3: 529 (1971>. Piper , D.W. and Heap , T .R .: Medical management of peptic ulcer with reference to anti-ulcer agents in other gastro-intestinal diseases. Drugs 3: 366 -403 (1972). Price, P.; Parkes, J .D . and Marsden, C.D.: Tiapride in Parkinson's disease . Lancet 2: 1106 (1978). Rao, N.S . and Pearce , J.: Amantadine in parkinsonism. An extended prospective trial . Practitioner 206 : 241-245 <1971>. Scherf, D.: Atropine in acute myocardial infarctions. American Heart Journal 86: 284 (1973). Schwab , R.S.; England , A.C .; Poskanzer, D.C. and Young , R.R .: American Medical Association 208 : 1168 (1969). Shealy , C.N .; Weeth, J .B. and Mercier, D.: Livedo reticularis in patients with parkinsonism receiving amantadine. Journal of the American Medical Association 212 : 1522-1523 (1970). Smith, S.E .: Mydriatic drugs for routine fundal infection . Lancet 2: 837-839 (1971>. 353 Tarsy, D.; Parkes , J.D . and Marsden, C.D. : Metoclopramide and pimozide in Parkinson's disease and levodopa-induced dyskinesias. Journal of Neurology, Neurosurgery and Psychiatry 38: 331-335 (1975). Teychenne, P.F.: Hepatocellular injury with distinctive metochondrial change s induced by lergotrile mesylate: A dopaminergic ergot derivative. Gastroenterology 76: 575-583 (1979). Tolosa, E.S.: Paradoxical suppression of chorea by apomorphine. Journal of the American Medical Assoc iation 229 : 1579-1580 (1974). Vitetta, M.: Effetti dell'amantadina sullo stato di viglanza nelle psicosindromi cerebrali diffuse vasculopatiche. Minerva Medica 62: 3984-3986 (1971>. Weiner, W,J .; Kramer, J.; Nausieda, P.A. and Klawans, H.L.: Paradoxical response to dopaminergic agents in Parkinsonism. Archives of Neurology 35: 453-455 (1978). Winer, J .A. and Bahn, S.: Loss of teeth with antidepressant drug therapy. Archives of General Psychiatry 16: 239-240 (1967) . Wood, B. and Haq , E.U.: An unusual case of atropine poisoning. British Journal of Clinical Practice 25: 469-470 (1971>. Author's address: Dr J.D. Parkes. University Department of Neurology, King's College Hospital, London SE5 (Eng1and).