ПОДДЕРЖИВАЮЩАЯ ТЕРАПИЯ ЭСЦИТАЛОПРАМОМ ДЛЯ
реклама

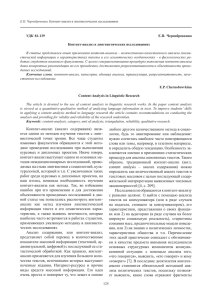
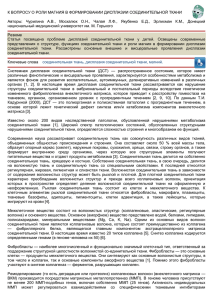
ÓÄÊ 616.895.4–085:65.214 ÏÎÄÄÅÐÆÈÂÀÞÙÀß ÒÅÐÀÏÈß ÝÑÖÈÒÀËÎÏÐÀÌÎÌ ÄËß ÏÐÅÄÎÒÂÐÀÙÅÍÈß ÐÅÊÓÐÐÅÍÒÍÎÉ ÄÅÏÐÅÑÑÈÈ: ÐÀÍÄÎÌÈÇÈÐÎÂÀÍÍÎÅ ÏËÀÖÅÁÎ-ÊÎÍÒÐÎËÈÐÓÅÌÎÅ ÈÑÑËÅÄÎÂÀÍÈÅ * Ñ. Ã. Êîðíøòåéí, A. Áîóç, Ä. Ëè, K. Ã. Ñàéêàëè, ×. Ãàíäè Áîëüøîå äåïðåññèâíîå ðàññòðîéñòâî (ÁÄÐ) êàê ðåêóððåíòíîå ñîñòîÿíèå â áîëüøèíñòâå ñëó÷àåâ ÿâëÿåòñÿ ïîæèçíåííûì çàáîëåâàíèåì (17, 19).  äëèòåëüíîì ïðîñïåêòèâíîì íàòóðàëèñòè÷åñêîì èññëåäîâàíèè, ïðîâåä¸ííîì â ðàìêàõ «Ïðîãðàììû ïî ïñèõîáèîëîãèè äåïðåññèè» â Íàöèîíàëüíîì èíñòèòóòå ïñèõè÷åñêîãî çäîðîâüÿ (ÑØÀ), áûëî ïîêàçàíî, ÷òî ïîñëå ðàçðåøåíèÿ äåïðåññèâíîãî ýïèçîäà, ðèñê ðàçâèòèÿ ðåöèäèâà â ïåðâûå 6 ìåñÿöåâ ñîñòàâëÿåò 30%, à â ïîñëåäóþùèå 12 ìåñÿöåâ – 40% (18). Ïðè ýòîì îòìå÷àëàñü íåîáõîäèìîñòü äëèòåëüíîé ïîääåðæèâàþùåé òåðàïèè (31).  îäíîì èç èññëåäîâàíèé, ïðîâåä¸ííîì â ÑØÀ çà áîëüíûìè áîëüøèì äåïðåññèâíûì ðàññòðîéñòâîì íàáëþäàëè íà ïðîòÿæåíèè 15 ëåò è ïðèøëè ê çàêëþ÷åíèþ, ÷òî ñóììàðíûé ðèñê ðàçâèòèÿ ðåöèäèâà çàáîëåâàíèÿ äîñòèãàåò 85% (29). Ïðè ýòîì ó ïàöèåíòîâ ñî ñòîéêîé ðåìèññèåé íà ïðîòÿæåíèè, ïî êðàéíåé ìåðå, 5 ëåò ñóììàðíûé ðèñê ðàçâèòèÿ ðåöèäèâà ñîñòàâèë 58%.  òî æå âðåìÿ, â äàííîì íàòóðàëèñòè÷åñêîì èññëåäîâàíèè êà÷åñòâî àíòèäåïðåññèâíîé òåðàïèè âî âðåìÿ ïåðâîãî ýïèçîäà è â ïîñëåäóþùåì áûëî íèçêèì. Ïî äàííûì ëèòåðàòóðû, ðèñê ðàçâèòèÿ ðåöèäèâà äåïðåññèè çàâèñèò îò êîëè÷åñòâà è äëèòåëüíîñòè ðàíåå ïåðåíåñ¸ííûõ ýïèçîäîâ (18, 36, 38). Çíà÷èìûì ïîêàçàòåëåì âîçìîæíîãî ðåöèäèâà çàáîëåâàíèÿ ÿâëÿåòñÿ íàëè÷èå ðåçèäóàëüíîé ñèìïòîìàòèêè ïîñëå ðàçðåøåíèÿ äåïðåññèâíîãî ýïèçîäà (16, 32).  ñâÿçè ñ ýòèì âåäåíèå äåïðåññèâíûõ ðàññòðîéñòâ äîëæíî âêëþ÷àòü äâå âàæíûå çàäà÷è – îáåñïå÷åíèå ëå÷åíèÿ, êîòîðîå ïðèâåä¸ò ïàöèåíòà ê ñîñòîÿíèþ çäîðîâüÿ è ïîääåðæàíèå ýòîãî ñîñòîÿíèÿ ñ ïîìîùüþ äëèòåëüíîé òåðàïèè.  ðàçëè÷íûõ èññëåäîâàíèÿõ áûëà ïðîäåìîíñòðèðîâàíà ïðîôèëàêòè÷åñêàÿ ýôôåêòèâíîñòü öåëîãî ðÿäà àíòèäåïðåññèâíûõ ñðåäñòâ ó áîëüíûõ ñ ðåêóððåíòíûì äåïðåññèâíûì ðàññòðîéñòâîì, âêëþ÷àÿ òðèöèêëè÷åñêèå àíòèäåïðåññàíòû èìèïðàìèí (8, 33) è íîðòðèïòèëèí (35), à òàêæå ôëóîêñåòèí (1, 26), ôëóâîêñàìèí (39), ïàðîêñåòèí (5, 7), ñåðòðàëèí (20, 23), öèòàëîïðàì (15) è âåíëàôàêñèí (27). Ýñöèòàëîïðàì – ñåëåêòèâíûé èíãèáèòîð îáðàòíîãî çàõâàòà ñåðîòîíèíà (ÑÈÎÇÑ), ñîñòîÿùèé öåëèêîì èç îäíîãî S-èçîìåðà, ïðîäåìîíñòðèðîâàë ñâîþ ýôôåêòèâíîñòü è õîðîøóþ ïåðåíîñèìîñòü ïðè êóïèðóþùåé òåðàïèè áîëüøîãî äåïðåññèâíîãî ðàññòðîéñòâà (4, 24, 41), à òàêæå â ïðåäîòâðàùåíèè ðàçâèòèÿ îáîñòðåíèé áîëüøèõ äåïðåññèâíûõ ýïèçîäîâ (34).  íàñòîÿùåì èññëåäîâàíèè èçó÷àëàñü ýôôåêòèâíîñòü ïîääåðæèâàþùåé òåðàïèè ýñöèòàëîïðàìîì ïðè ïðîôèëàêòèêå ðàçâèòèÿ ðåöèäèâîâ äåïðåññèè ó ïàöèåíòîâ, ïîëîæèòåëüíî ðåàãèðîâàâøèõ íà òåðàïèþ äðóãèì àíòèäåïðåññàíòîì èç ãðóïïû ÑÈÎÇÑ. Âàæíî îòìåòèòü, ÷òî ýôôåêòèâíîñòü ïîääåðæèâàþùåé òåðàïèè ýñöèòàëîïðàìîì èçó÷àëàñü ó ïàöèåíòîâðåñïîíäåðîâ íà äðóãîé àíòèäåïðåññàíò èç ãðóïïû ÑÈÎÇÑ â êóïèðóþùåé ôàçå ëå÷åíèÿ, ÷òî îòëè÷àåò äàííîå èññëåäîâàíèå îò òåõ (23), ãäå ïðîôèëàêòè÷åñêàÿ òåðàïèÿ ïðîäîëæàëàñü òåì æå ïðåïàðàòîì. Ìåòîäû Íàñòîÿùåå èññëåäîâàíèå áûëî ïðîâåäåíî â 3 ýòàïà: (1) îòêðûòàÿ êóïèðóþùàÿ ôàçà ëå÷åíèÿ; (2) îòêðûòàÿ ñòàáèëèçèðóþùàÿ ôàçà ëå÷åíèÿ; (3) ðàíäîìèçèðîâàííîå äâîéíîå ñëåïîå ïëàöåáî-êîíòðîëèðóåìîå èññëåäîâàíèå ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ. Èññëåäîâàíèå ïðîâîäèëîñü íà áàçå 28 êëèíè÷åñêèõ öåíòðîâ â ÑØÀ. Ïàöèåíòû áûëè âêëþ÷åíû âî âòîðîé ýòàï èññëåäîâàíèÿ ïî çàâåðøåíèè îñòðîé ôàçû çàáîëåâàíèÿ. Ïî ðåçóëüòàòàì òåðàïèè íà ýòîì ýòàïå âñå ïàöèåíòû ðàçäåëåíû íà 3 ãðóïïû.  íàñòîÿùåì ñîîáùåíèè ïðèâîäÿòñÿ äàííûå òîëüêî î ïàöèåíòàõ-ðåñïîíäåðàõ íà òåðàïèþ ÑÈÎÇÑ â îñòðîé ôàçå çàáîëåâàíèÿ è ïðîäîëæèâøèõ òåðàïèþ â ñòàáèëèçèðóþùåé ôàçå ëå÷åíèÿ. Ïîëíàÿ èíôîðìàöèÿ î äàííûõ èññëåäîâàíèÿ äîñòóïíà â «Ðåãèñòðå êëèíè÷åñêèõ èññëåäîâàíèé» êîìïàíèè Forest Laboratories (6). Âûáîðêà, âîøåäøàÿ â èññëåäîâàíèå.  èññëåäîâàíèå áûëè âêëþ÷åíû ïàöèåíòû (ìóæ. è æåí. â âîçðàñòå 18–81 ãîäà) ñ äèàãíîçîì áîëüøîãî äåïðåñ- * Ðàñøèðåííûé ðåôåðàò ñòàòüè, îïóáëèêîâàííîé â J. Clin. Psychiatry. – 2006. – Vol. 67. – P. 1767–1775, ïðåäîñòàâëåí äëÿ ïóáëèêàöèè êîìïàíèåé Ëóíäáåê. 79 ñèâíîãî ðàññòðîéñòâà ïî DSM-IV â îñòðîé ôàçå, äëèòåëüíîñòüþ ñîñòîÿíèÿ íå ìåíåå 4-õ íåäåëü è, ïî êðàéíåé ìåðå, ñ äâóìÿ áîëüøèìè äåïðåññèâíûìè ýïèçîäàìè â àíàìíåçå, îäèí èç êîòîðûõ íàáëþäàëñÿ â òå÷åíèå ïîñëåäíèõ 5 ëåò. Òÿæåñòü çàáîëåâàíèÿ ñîñòàâëÿëà íå ìåíåå 22 áàëëîâ ïî øêàëå îöåíêè äåïðåññèè Ìîíòãîìåðè-Àñáåðã (MADRS), ïðè ýòîì îöåíêà ïî 1 ïóíêòó øêàëû äåïðåññèè Ãàìèëüòîíà (HAM-D) äîëæíà áûëà ñîñòàâëÿòü ìèíèìóì 2 áàëëà. Ïàöèåíòû äîëæíû áûëè áûòü ñîìàòè÷åñêè çäîðîâû èëè èìåòü êëèíè÷åñêè íåçíà÷èìûå èçìåíåíèÿ ïî äàííûì ñîìàòè÷åñêîãî îáñëåäîâàíèÿ, ëàáîðàòîðíûõ è ÝÊà ïîêàçàòåëåé.  èññëåäîâàíèå íå âêëþ÷àëè ïàöèåíòîâ ñ äèàãíîçîì áèïîëÿðíîãî ðàññòðîéñòâà, øèçîôðåíèè èëè äðóãîãî ïñèõîòè÷åñêîãî ðàññòðîéñòâà, îáñåññèâíîêîìïóëüñèâíîãî ðàññòðîéñòâà, óìñòâåííîé îòñòàëîñòè, êîãíèòèâíîãî ðàññòðîéñòâà. Áûëè èñêëþ÷åíû ïàöèåíòû, äèàãíîç êîòîðûõ ñîîòâåòñòâîâàë ëþáîìó çàáîëåâàíèþ Îñè I DSM-IV, êðîìå áîëüøîãî äåïðåññèâíîãî ðàññòðîéñòâà (âêëþ÷àÿ äèñòèìèþ), èìåâøèå â àíàìíåçå ëþáîå ïñèõîòè÷åñêîå ðàññòðîéñòâî, äåìîíñòðèðîâàâøèå ïñèõîòè÷åñêóþ ñèìïòîìàòèêó, ñ âûðàæåííûì ðàññòðîéñòâîì ëè÷íîñòè, ñî çëîóïîòðåáëåíèåì ïñèõîàêòèâíûìè âåùåñòâàìè â òå÷åíèå ïîñëåäíèõ 6 ìåñÿöåâ. Òàêæå â èññëåäîâàíèå íå áûëè âêëþ÷åíû ïàöèåíòû ñ âûñîêèì ñóèöèäàëüíûì ðèñêîì, ñîñòîÿíèå êîòîðûõ îöåíèâàëîñü ìèíèìóì â 5 áàëëîâ ïî 10 ïóíêòó øêàëû MADRS (ñóèöèäàëüíûå òåíäåíöèè), èëè íóæäàâøèåñÿ â äîïîëíèòåëüíîé ïñèõîòðîïíîé òåðàïèè (çà èñêëþ÷åíèåì çîëïèäåìà, äëÿ êóïèðîâàíèÿ èíñîìíèè). Äèçàéí èññëåäîâàíèÿ. Íà ýòàïå êóïèðóþùåé ôàçû ëå÷åíèÿ â îòêðûòîì 8-íåäåëüíîì èññëåäîâàíèè ïà- öèåíòû ïîëó÷àëè â ãèáêîé äîçèðîâêå îäèí èç ñëåäóþùèõ ïðåïàðàòîâ: öèòàëîïðàì (20–60 ìã/ñóò), ôëóîêñåòèí (20–80 ìã/ñóò), ïàðîêñåòèí (20–50 ìã/ ñóò) èëè ñåðòðàëèí (50–200 ìã/ñóò) (ðèñ. 1) (42). Ðåñïîíäåðû (MADRS≤12 áàëëîâ) íà òåðàïèþ îäíèì èç ÑÈÎÇÑ â êóïèðóþùåé ôàçå ëå÷åíèÿ âêëþ÷àëèñü âî âòîðóþ ôàçó èññëåäîâàíèÿ.  îòêðûòîì èññëåäîâàíèè ñòàáèëèçèðóþùåé ôàçû òåðàïèè ïàöèåíòàì-ðåñïîíäåðàì èç ïåðâîé ôàçû, íàçíà÷àëñÿ ýñöèòàëîïðàì â ãèáêîé äîçèðîâêå. Ëå÷åíèå ýñöèòàëîïðàìîì íà÷èíàëîñü â òå÷åíèå ïåðâûõ 72 ÷àñîâ ïîñëå îêîí÷àíèÿ ïåðâîé ôàçû òåðàïèè, ïðè ýòîì äîçà ïðåïàðàòà ñîñòàâëÿëà 10 ìã/ ñóò.  ñîîòâåòñòâèè ñ ðåøåíèåì èññëåäîâàòåëÿ, äîçà ïðåïàðàòà ìîãëà áûòü ïîâûøåíà äî 20 ìã/ñóò, íà÷èíàÿ ñ êîíöà ïåðâîé íåäåëè òåðàïèè. Ïî çàâåðøåíèè ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ, ïàöèåíòû, îñòàâàâøèåñÿ ðåñïîíäåðàìè (MADRS≤12 áàëëîâ), äîïóñêàëèñü ê ïðîäîëæåíèþ òåðàïèè â 52-íåäåëüíîì ðàíäîìèçèðîâàííîì äâîéíîì ñëåïîì ïëàöåáîêîíòðîëèðóåìîì èññëåäîâàíèè ïîääåðæèâàþùåé òåðàïèè ñ ïàðàëëåëüíûìè ãðóïïàìè è ôèêñèðîâàííûìè äîçàìè ïðåïàðàòà. Ïàöèåíòû, íå ñîîòâåòñòâîâàâøèå êðèòåðèÿì ðåñïîíäåðîâ ê êîíöó ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ, áûëè èñêëþ÷åíû èç èññëåäîâàíèÿ. Ïàöèåíòû, äîïóùåííûå ê òðåòüåìó ýòàïó èññëåäîâàíèÿ, áûëè ðàíäîìèçèðîâàíû (òî åñòü ðàñïðåäåëåíû ñëó÷àéíûì îáðàçîì) â îäíó èç äâóõ òåðàïåâòè÷åñêèõ ãðóïï – ïëàöåáî èëè ýñöèòàëîïðàìà â ñîîòíîøåíèè 1:1. Íå äîïóñêàëèñü êàêèå-ëèáî èçìåíåíèÿ â êîëè÷åñòâå ïðèíèìàåìîãî ïðåïàðàòà â ñóòêè. Ðåöèäèâ äåïðåññèè îïðåäåëÿëñÿ ïðè óâåëè÷åíèè îöåíêè ïî Ðèñ. 1. Äèçàéí èññëåäîâàíèÿ Ïðèìå÷àíèå: *MADRS – øêàëà Ìîíòãîìåðè-Àñáåðã äëÿ îöåíêè äåïðåññèè 80 øêàëå MADRS≤22 áàëëîâ èëè âûáûòèè èç èññëåäîâàíèÿ â ñâÿçè ñ ðåøåíèåì èññëåäîâàòåëÿ î íåäîñòàòî÷íîé ýôôåêòèâíîñòè òåðàïèè. Ïàöèåíòû, ÷ü¸ ñîñòîÿíèå îöåíèâàëîñü êàê ðåöèäèâ çàáîëåâàíèÿ âî âðåìÿ îäíîãî èç âèçèòîâ ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ, áûëè èñêëþ÷åíû èç èññëåäîâàíèÿ. Îöåíêó ñîñòîÿíèÿ ïàöèåíòîâ ïðîâîäèëè â êîíöå 1, 2, 4, 8 è êàæäûõ ïîñëåäóþùèõ 4 íåäåëü â òå÷åíèå ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ, à òàêæå â êîíöå 18, 20 è êàæäîé ïîñëåäóþùåé 4 íåäåëè âî âðåìÿ ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ. Îöåíêà ïðîâîäèëàñü ñ èñïîëüçîâàíèåì øêàë MADRS, HAMD-24, ïîäøêàë «Óëó÷øåíèå» (CGI-I) è «Òÿæåñòü çàáîëåâàíèÿ» (CGI-S) øêàëû îáùåãî êëèíè÷åñêîãî âïå÷àòëåíèÿ (12). Ïîêàçàòåëè áåçîïàñíîñòè îöåíèâàëèñü ñ ïîìîùüþ ìîíèòîðèðîâàíèÿ âèòàëüíûõ ôóíêöèé è ïîáî÷íûõ ýôôåêòîâ. Ïîáî÷íûå ýôôåêòû, ïðîÿâèâøèåñÿ âî âðåìÿ ëþáîé ôàçû èññëåäîâàíèÿ, îïðåäåëÿëèñü êàê íåæåëàòåëüíûå ÿâëåíèÿ â ðåçóëüòàòå òåðàïèè, åñëè îíè îòñóòñòâîâàëè íà ìîìåíò âêëþ÷åíèÿ â èññëåäîâàíèå èëè æå åñëè èìåëè ìåñòî, íî óòÿæåëèëèñü âî âðåìÿ òåðàïèè. Ôèçèêàëüíîå îáñëåäîâàíèå è ëàáîðàòîðíûå òåñòû ïðîâîäèëèñü âî âðåìÿ ïåðâîãî âèçèòà è â êîíöå èññëåäîâàíèÿ; îöåíêà ëàáîðàòîðíûõ ïîêàçàòåëåé ïðîâîäèëàñü òàêæå è íà 12 íåäåëå ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ. Ïàðàìåòðû ýëåêòðîêàðäèîãðàììû îöåíèâàëèñü â êîíöå 12 íåäåëè ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ è â êîíöå èññëåäîâàíèÿ. Ñòàòèñòè÷åñêèå ìåòîäû. Àíàëèç ïîêàçàòåëåé áåçîïàñíîñòè áûë îñíîâàí íà ìàòåðèàëå âûáîðêè ïàöèåíòîâ, ïîëó÷èâøèõ òåðàïèþ ìèíèìóì 1 ðàç â òå÷åíèå ñòàáèëèçèðóþùåé èëè ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ. Îáùàÿ âûáîðêà (intention-to-treat population, ITT âûáîðêà) âêëþ÷àëà âñåõ ïàöèåíòîâ, ïîëó÷èâøèõ, ïî ìåíüøåé ìåðå, îäíó äîçó èçó÷àåìîãî ïðåïàðàòà è èìåâøèõ õîòÿ áû îäíîêðàòíî çàôèêñèðîâàííûå ïîêàçàòåëè ïî øêàëå MADRS â ñòàáèëèçèðóþùåé èëè ïîääåðæèâàþùåé ôàçàõ èññëåäîâàíèÿ, ñäåëàííûå ïîñëå îïðåäåëåíèÿ áàçèñíûõ çíà÷åíèé ýòîé øêàëû â íà÷àëå êàæäîé ôàçû. Çà íà÷àëî ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ áûë ïðèíÿò ïîñëåäíèé îöåíî÷íûé âèçèò âî âðåìÿ êóïèðóþùåé ôàçû òåðàïèè. Çà íà÷àëî ïîääåðæèâàþùåé ôàçû ïðèíÿò ïîñëåäíèé îöåíî÷íûé âèçèò âî âðåìÿ ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ. Ñðàâíèìîñòü íåïðåðûâ- íûõ ïåðåìåííûõ âåëè÷èí ìåæäó äâóìÿ ãðóïïàìè íà èñõîäå ïîääåðæèâàþùåé òåðàïèè àíàëèçèðîâàëàñü ñ ïðèìåíåíèåì ìîäåëè äâóñòîðîííåãî âàðèàöèîííîãî àíàëèçà, êàòåãîðèàëüíûå âåëè÷èíû àíàëèçèðîâàëè òåñòîì Cochran-Mantel-Haenszel. Ãëàâíûì ïîêàçàòåëåì ýôôåêòèâíîñòè áûëî âðåìÿ äî ðàçâèòèÿ ðåöèäèâà îò íà÷àëà äâîéíîé ñëåïîé ïîääåðæèâàþùåé ôàçû èññëåäîâàíèÿ. Ñðàâíåíèå ðèñêà ðàçâèòèÿ ðåöèäèâà â ãðóïïå ïàöèåíòîâ, ïîëó÷àþùèõ ýñöèòàëîïðàì è ïëàöåáî, îöåíèâàëîñü ñ ïîìîùüþ ìîäåëè ðåãðåññèè Êîêñà. Áûë ïðèìåí¸í òàêæå àíàëèç âûæèâàåìîñòè Kaplan-Meier. Äëÿ ïàðíûõ ñðàâíåíèé ìåæäó òåðàïåâòè÷åñêèìè ãðóïïàìè (ýñöèòàëîïðàì, ïëàöåáî) ñ ó÷¸òîì ïàðàìåòðîâ ýôôåêòèâíîñòè (èçìåíåíèÿ ìåæäó èñõîäíûìè è êîíå÷íûìè çíà÷åíèÿìè) áûëà èñïîëüçîâàíà ìîäåëü äîïîëíèòåëüíîãî êîâàðèàöèîííîãî àíàëèçà. Ðåçóëüòàòû Õàðàêòåðèñòèêà ïàöèåíòîâ. Âñåãî â îòêðûòóþ êóïèðóþùóþ ôàçó ëå÷åíèÿ áûëî âêëþ÷åíî 515 ïàöèåíòîâ (ñðåäíèé áàëë ïî MADRS – 30,4); 386 ïàöèåíòîâ (75%) çàâåðøèëè ýòîò ýòàï, ïðè ýòîì 259 (50%) îêàçàëèñü ðåñïîíäåðàìè. Âñåãî 234 ïàöèåíòà-ðåñïîíäåðà íà òåðàïèþ ÑÈÎÇÑ â êóïèðóþùåé ôàçå ëå÷åíèÿ ïîëó÷àëè, êàê ìèíèìóì, 1 äîçó ýñöèòàëîïðàìà âî âðåìÿ ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ (ðèñ. 2). Ñòî øåñòüäåñÿò ÷åòûðå (70%) ïàöèåíòà èç ýòîé ãðóïïû çàâåðøèëè ýòàï ñòàáèëèçèðóþùåãî ëå÷åíèÿ, 139 ïàöèåíòîâ ïîëó÷èëè, ïî êðàéíåé ìåðå, 1 äîçó ïðåïàðàòà âî âðåìÿ äâîéíîãî ñëåïîãî èññëåäîâàíèÿ ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ; èç íèõ 73 ïðèíèìàëè ýñöèòàëîïðàì è 66 – ïëàöåáî. Ýòè ïàöèåíòû áûëè âêëþ÷åíû â àíàëèç áåçîïàñíîñòè ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ.  ITT âûáîðêó (ñ ìèíèìóì îäíîé îöåíêîé ïî øêàëå MADRS) â ïîääåðæèâàþùåé ôàçå ëå÷åíèÿ âîøëî 73 ïàöèåíòà, ïîëó÷àâøèõ ýñöèòàëîïðàì, è 65 ïàöèåíòîâ, ïîëó÷àâøèõ ïëàöåáî. Ïîääåðæèâàþùóþ 52-íåäåëüíóþ ôàçó ëå÷åíèÿ çàâåðøèëè 49 ïàöèåíòîâ (35%): 37 (51%) èç ãðóïïû, ïîëó÷àâøèõ ýñöèòàëîïðàì, è 12 (18%) èç ãðóïïû, ïîëó÷àâøèõ ïëàöåáî. Ïîñëå ðàíäîìèçàöèè â äâîéíîì ñëåïîì èññëåäîâàíèè ãðóïïû íå îáíàðóæèâàëè ñòàòèñòè÷åñêè äîñòîâåðíûõ ðàçëè÷èé ïî âîçðàñòó, ïîëó è êëèíè÷åñêèì ïîêàçàòåëÿì (òàáë. 1). Ñðåäíÿÿ ñóòî÷íàÿ äîçà ýñöèòàÒàáëèöà 1 Демографическая характеристика пациентов* Õàðàêòåðèñòèêà Ñòàáèëèçèðóþùàÿ ôàçà, îòêðûòîå èññëåäîâàíèå Ïîääåðæèâàþùàÿ ôàçà, äâîéíîå ñëåïîå èññëåäîâàíèå Ýñöèòàëîïðàì(n=234) Ýñöèòàëîïðàì (n=73) Ïëàöåáî(n=66) Âîçðàñò, ãîäû 40,5±11,6 42,0±11,3 43,7±12,4 Æåíùèíû (%) 175 (74,8) 58 (79,5) 52 (78,8) Ðàñà, % áåëûõ 196 (83,8) 64 (87,7) 57 (86,4) Êîëè÷åñòâî áàëëîâ ïî øêàëå MADRS** íà íà÷àëî èññëåäîâàíèÿ 6,6±3,4 4,7±4,0 4,9±3,6 Êîëè÷åñòâî äåïðåññèâíûõ ýïèçîäîâ â àíàìíåçå 4,8±3,9 4,7±3,1 5,8±6,0 Ïðèìå÷àíèå: * – çíà÷åíèÿ ïðåäñòàâëåíû êàê ñðåäíåå ± SD (ñòàíäàðòíîå îòêëîíåíèå) ïðè îòñóòñòâèè èíûõ óêàçàíèé; **MADRS – øêàëà Ìîíòãîìåðè-Àñáåðã äëÿ îöåíêè äåïðåññèè. 81 Ðèñ. 2. Ðàñïðåäåëåíèå ïàöèåíòîâ Ïðèìå÷àíèå: *Safety – âûáîðêà ïàöèåíòîâ, ïîëó÷èâøàÿ, ïî êðàéíåé ìåðå, 1 äîçó ïðåïàðàòà (âîøëè â àíàëèç áåçîïàñíîñòè); **ITT – intention-to-treat population – âûáîðêà ïàöèåíòîâ, ñ ìèíèìóì îäíîé îöåíêîé ïî øêàëå MADRS ïîñëå ðåãèñòðàöèè èñõîäíûõ ïîêàçàòåëåé (âîøëè â àíàëèç ýôôåêòèâíîñòè). ëîïðàìà âî âðåìÿ îòêðûòîé ñòàáèëèçèðóþùåé ôàçû è äâîéíîé ñëåïîé ïîääåðæèâàþùåé ôàçû èññëåäîâàíèÿ ñîñòàâèëà 15,8 ìã è 15,2 ìã ñîîòâåòñòâåííî. Ïðåäîòâðàùåíèå ðåöèäèâîâ äåïðåññèè. Íà íà÷àëî ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ ñðåäíÿÿ îöåíêà ïî ãðóïïå ñîñòàâëÿëà 6,6±3,4 áàëëà ïî øêàëå MADRS. Íà íà÷àëî ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ îöåíêà ïî MADRS ñîñòàâèëà 4,9±3,6 áàëëîâ â ãðóïïå ïëàöåáî è 4,7±4,0 äëÿ ïàöèåíòîâ, ðàíäîìèçèðîâàííûõ â ãðóïïó ýñöèòàëîïðàìà. Ñðåäíèå èçìåíåíèÿ ñóììàðíûõ áàëëîâ øêàë MADRS, HAM-D, CGI-I, CGI-S â ïåðèîä ñòàáèëèçèðóþùåé è ïîääåðæèâàþùåé ôàç ëå÷åíèÿ ïðåäñòàâëåíû â òàáë. 2. Êóìóëÿòèâíàÿ ÷àñòîòà ðàçâèòèÿ ðåöèäèâà äåïðåññèè áûëà çíà÷èòåëüíî íèæå ó ïàöèåíòîâ, ïðèíèìàâøèõ ýñöèòàëîïðàì â ñðàâíåíèè ñ ãðóïïîé ïëàöåáî (27% è 65% ñîîòâåòñòâåííî). Ïðè ýòîì â ãðóïïå ýñöèòàëîïðàìà äî ðàçâèòèÿ ðåöèäèâà ïðîõîäèëî äîñòîâåðíî (p<0,001) áîëüøå âðåìåíè (252±134 äíÿ), ÷åì ó ïàöèåíòîâ, ïîëó÷àâøèõ ïëàöåáî (130±135 äíåé) (òàáë. 3). Àíàëèç áûë ïðîâåäåí òàêæå ïîñëå ó÷åòà âñåõ ðåöèäèâîâ çàáîëåâàíèÿ â òå÷åíèå 14 äíåé ïîñëå íà÷àëà äâîéíîãî ñëåïîãî èññëåäîâàíèÿ. Ðåçóëüòàòû îñòàâàëèñü ñòàòèñòè÷åñêè çíà÷èìûìè (îòíîøåíèå ðèñêîâ ÎÐ=0,29; p<0,001) â ïîëüçó òåðàïèè ýñöèòàëîïðàìîì. Áåçîïàñíîñòü. Òåðàïèÿ ýñöèòàëîïðàìîì â ñòàáèëèçèðóþùåé è ïîääåðæèâàþùåé ôàçàõ ëå÷åíèÿ áûëà áåçîïàñíîé è õîðîøî ïåðåíîñèëàñü ïàöèåíòàìè.  ñòàáèëèçèðóþùåé ôàçå èññëåäîâàíèÿ ÷àñòîòà ïðåæäåâðåìåííîé îòìåíû òåðàïèè èç-çà íåæåëàòåëüíûõ ÿâëåíèé ïðè ïðèåìå ýñöèòàëîïðàìà ñîñòàâèëà 6%. Âî âðåìÿ ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ ÷àñòîòà ïðåæäåâðåìåííîé îòìåíû èç-çà íåæåëàòåëüíûõ ÿâëåíèé ïðè ïðèåìå ýñöèòàëîïðàìà (4%) áûëà äàæå íåñêîëüêî íèæå, ÷åì ïðè èñïîëüçîâàíèè ïëàöåáî (9%) (ðèñ. 2). Åäèíñòâåííûìè íåæåëàòåëüíûìè ÿâëåíèÿìè â ñâÿçè ñ òåðàïèåé ýñöèòàëîïðàìîì â îòêðûòîé ôàçå èññëåäîâàíèÿ, íàáëþäàâøèåñÿ â ≤10% ñëó÷àåâ, áûëè ãîëîâíàÿ áîëü è óòîìëÿåìîñòü. ×àñòîòà ðàçâèòèÿ òàêèõ íåæåëàòåëüíûõ ÿâëåíèé êàê ãîëîâîêðóæåíèå, ãðèïïîïîäîáíûå ñèìïòîìû, èíôåêöèè âåðõíèõ äûõàòåëüíûõ ïóòåé, ðèíèòû è ãîëîâíûå áîëè áûëà ïðèìåðíî îäèíàêîâîé (≥10%) â ãðóïïàõ ýñöèòàëîïðàìà è ïëàöåáî â 82 Òàáëèöà 2 Дополнительные параметры эффективности: открытая стабилизирующая фаза и двойная слепая поддерживающая фаза (ITT выборка, OC) Ïàðàìåòð ýôôåêòèâíîñòè Ñòàáèëèçèðóþùàÿ ôàçà, îòêðûòîå èññëåäîâàíèå Ïîääåðæèâàþùàÿ ôàçà, äâîéíîå ñëåïîå èññëåäîâàíèå Ýñöèòàëîïðàì (n=228) Ýñöèòàëîïðàì (n=73) Ïëàöåáî (n=65) 6,6±3,4 4,7±4,0 4,9±3,6 -0,3±0,49 0,1±5,8 -0,3±3,0 MADRS íà÷àëî èññëåäîâàíèÿ çàâåðøåíèå èññëåäîâàíèÿ HAM-D íà÷àëî èññëåäîâàíèÿ çàâåðøåíèå èññëåäîâàíèÿ 7,2±4,1 5,2±4,0 5,2±3,8 -0,3±0,48 -0,5±5,9 -0,2±3,6 CGI-I íà÷àëî èññëåäîâàíèÿ 1,4±0,5 1,2±0,5 1,2±0,4 çàâåðøåíèå èññëåäîâàíèÿ 0,0±0,8 0,0±0,6 -0,1±0,3 íà÷àëî èññëåäîâàíèÿ 1,9±0,7 1,5±0,6 1,6±0,7 çàâåðøåíèå èññëåäîâàíèÿ 0,1±1,2 0,0±0,9 0,1±0,3 CGI-S Ïðèìå÷àíèå: * CGI-I – øêàëà îáùåãî êëèíè÷åñêîãî âïå÷àòëåíèÿ, ïîäøêàëà «Óëó÷øåíèå», CGI-S – øêàëà îáùåãî êëèíè÷åñêîãî âïå÷àòëåíèÿ, ïîäøêàëà «Òÿæåñòü çàáîëåâàíèÿ», HAM-D – øêàëà îöåíêè äåïðåññèè Ãàìèëüòîíà, MADRS – øêàëà îöåíêè äåïðåññèè Ìîíòãîìåðè-Àñáåðã, ITT – intention-to-treat population – âûáîðêà ïàöèåíòîâ, ñ ìèíèìóì îäíîé îöåíêîé ïî øêàëå MADRS ïîñëå ðåãèñòðàöèè èñõîäíûõ ïîêàçàòåëåé, OC – observed cases – íàáëþäàåìûå ñëó÷àè Òàáëèöà 3 Суммарный риск развития рецидива депрессии (ITT выборка) Ñóììàðíûé ðèñê ðåöèäèâà 95% ÄÈ p Áåç êîððåêöèè Ýñöèòàëîïðàì (n=73) Ïëàöåáî (n=65) Îòíîøåíèå ðèñêîâ 27% 65% 0,26 0,13 ê 0,52 <0,001 Ñ êîððåêöèåé ðåöèäèâîâ â òå÷åíèå ïåðâûõ 14 äíåé äâîéíîãî ñëåïîãî ïåðèîäà 27% 62% 0,29 0,14 ê 0,59 <0,001 Ïðèìå÷àíèå: *ITT – intention-to-treat population – âûáîðêà ïàöèåíòîâ, ñ ìèíèìóì îäíîé îöåíêîé ïî øêàëå MADRS ïîñëå ðåãèñòðàöèè èñõîäíûõ ïîêàçàòåëåé (âîøëè â àíàëèç ýôôåêòèâíîñòè) Òàáëèöà 4 Наиболее частые побочные эффекты, связанные с терапией, в период двойной слепой фазы поддерживающего лечения, %* Ïîáî÷íûé ýôôåêò, ñâÿçàííûé ñ ïðè¸ìîì òåðàïèè Ýñöèòàëîïðàì (n=73) Ïëàöåáî (n=66) p 3 20 0,002 Ãîëîâîêðóæåíèå Ãðèïïîïîäîáíûå ñèìïòîìû 16 2 0,003 Èíôåêöèè âåðõíèõ äûõàòåëüíûõ ïóòåé 16 12 0,629 Óøèáû 12 5 0,135 Ðèíèòû 11 9 0,783 Ãîëîâíàÿ áîëü 11 6 0,374 Ïðèìå÷àíèå: * – ÷àñòîòà íå ìåíåå 10% â îáåèõ òåðàïåâòè÷åñêèõ ãðóïïàõ. äâîéíîé ñëåïîé ïîääåðæèâàþùåé ôàçå èññëåäîâàíèÿ (òàáë. 4).  òå÷åíèå ïåðâûõ 14 äíåé ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ ÷àñòîòà íåæåëàòåëüíûõ ÿâëåíèé ñîñòàâèëà 41% â ãðóïïå, ïîëó÷àâøèõ ïëàöåáî, è 21% – â ãðóïïå, ïîëó÷àâøèõ ýñöèòàëîïðàì (òàáë. 5). Ãîëîâîêðóæåíèå, íàèáîëåå òèïè÷íîå íåæåëàòåëüíîå ÿâëåíèå, âîçíèêàþùåå ïðè îòìåíå ÑÈÎÇÑ, ïðèöåëüíî îòñëåæèâàëîñü â òå÷åíèå ïåðâûõ 14 äíåé ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ.  ãðóïïå èç 66 ïàöèåíòîâ, ïîëó÷àâøèõ ïëàöåáî, íà êîòîðîå îíè áûëè ïåðåâåäåíû ïîñëå ïîëó÷åíèÿ ýñöèòàëîïðàìà â îòêðûòîé ôàçå ñòàáèëèçèðóþùåãî ëå÷åíèÿ, 12 (18%) èñïûòûâàëè ãîëîâîêðóæåíèå â òå÷åíèå ïåðâûõ 14 äíåé ëå÷åíèÿ. Âñëåä çà ýòèì ïåðèîäîì ÷àñ- òîòà ðàçâèòèÿ ãîëîâîêðóæåíèÿ ó ïàöèåíòîâ ýòîé ãðóïïû ñîñòàâèëà 2%.  ãðóïïå ïàöèåíòîâ, ïîëó÷àâøèõ ýñöèòàëîïðàì, íèêòî íå èñïûòûâàë ãîëîâîêðóæåíèå â òå÷åíèå ïåðâûõ 14 äíåé ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ, â òî âðåìÿ êàê â ïîñëåäóþùåì ïåðèîäå ÷àñòîòà âîçíèêíîâåíèÿ ýòîãî íåæåëàòåëüíîãî ÿâëåíèÿ ñîñòàâèëà 3%. Ñåðü¸çíûå íåæåëàòåëüíûå ÿâëåíèÿ â òå÷åíèå ñòàáèëèçèðóþùåé ôàçû ëå÷åíèÿ íå íàáëþäàëèñü. Ñîîáùàëîñü î 4 ñåðü¸çíûõ íåæåëàòåëüíûõ ÿâëåíèÿõ ó òð¸õ ïàöèåíòîâ â ïåðèîä ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ (ó 1 â ãðóïïå ïëàöåáî – ñóèöèäàëüíàÿ ïîïûòêà; è ó 2 â ãðóïïå ýñöèòàëîïðàìà – ñëó÷àé ãèïîòåíçèè; îïóùåíèå ìî÷åâîãî ïóçûðÿ è îïóùåíèå ìàòêè). Òåì íå ìåíåå, íè îäíî èç ýòèõ ñåðü¸çíûõ 83 Òàáëèöà 5 Частота возникновения побочных эффектов, связанных с приёмом терапии в течение первых 14 дней двойной слепой фазы поддерживающего лечения, %* Ïîáî÷íûé ýôôåêò, ñâÿçàííûé ñ ïðè¸ìîì òåðàïèè Ýñöèòàëîïðàì Ïëàöåáî (n=73) (n=66) Ãîëîâîêðóæåíèå 0 18,2 Ðèíèòû 0 6,1 Èíôåêöèè âåðõíèõ äûõàòåëüíûõ ïóòåé 0 3,0 1,4 1,5 Óøèáû 2,7 1,5 Ãðèïïîïîäîáíûå ñèìïòîìû 1,4 0 Ãîëîâíûå áîëè ìîãî âëèÿíèÿ íà âåñ â îáåèõ òåðàïåâòè÷åñêèõ ãðóïïàõ ñðåäè ïàöèåíòîâ, çàâåðøèâøèõ ïîääåðæèâàþùóþ ôàçó ëå÷åíèÿ. Îáñóæäåíèå Ïðîâåä¸ííîå èññëåäîâàíèå äåìîíñòðèðóåò, ÷òî ïîääåðæèâàþùàÿ òåðàïèÿ ýñöèòàëîïðàìîì áåçîïàñíà, õîðîøî ïåðåíîñèòñÿ è çíà÷èòåëüíî ñíèæàåò ðèñê ðåöèäèâà äåïðåññèâíîãî ðàññòðîéñòâà. Áûëî ïîêàçàíî, ÷òî ó ïàöèåíòîâ, ïðèíèìàâøèõ ýñöèòàëîïðàì â ñðàâíåíèè ñ òåìè, êòî ïîëó÷àë ïëàöåáî, ñóììàðíûé ðèñê ðàçâèòèÿ ðåöèäèâà áûë â 2,5 ðàçà íèæå (27% ðåöèäèâîâ â ãðóïïå ýñöèòàëîïðàìà è 67% â ãðóïïå ïëàöåáî). Ïðè ýòîì äî ðàçâèòèÿ ðåöèäèâà çàáîëåâàíèÿ â ãðóïïå ýñöèòàëîïðàìà (â òåõ íåìíîãèõ ñëó÷àÿõ, êîãäà îí âîçíèêàë) ïðîõîäèëî çíà÷èòåëüíî áîëüøå âðåìåíè, ÷åì äî ðàçâèòèÿ ðåöèäèâà íà ïëàöåáî. Ñèìïòîìû îòìåíû, íàáëþäàåìûå â ñâÿçè ñ ïðåêðàùåíèåì ïðè¸ìà àêòèâíîãî ïðåïàðàòà ó ïàöèåíòîâ èç ãðóïïû ïëàöåáî, íå ïîâëèÿëè íà îêîí÷àòåëüíûå ðåçóëüòàòû ñðàâíåíèÿ, ïîñêîëüêó ïðèìåíÿëñÿ ñïåöèàëüíûé ìåòîä êîððåêòèðîâêè äàííûõ.  îäíîì èç ïðåäûäóùèõ èññëåäîâàíèé áûëà ïîêàçàíà ýôôåêòèâíîñòü ýñöèòàëîïðàìà ïî ïðåäóïðåæäåíèþ ðàçâèòèÿ ðåöèäèâîâ äåïðåññèè ïðè ïðèìåíåíèè åãî â êà÷åñòâå ñòàáèëèçèðóþùåé òåðàïèè â òå÷åíèå 36 íåäåëü (34).  íàñòîÿùåì èññëåäîâàíèè ðàññìàòðèâàåòñÿ ýôôåêòèâíîñòü èñïîëüçîâàíèÿ ýñöèòàëîïðàìà â ïîääåðæèâàþùåé ôàçå ëå÷åíèÿ. Ìíîãèìè àíòèäåïðåññàíòàìè, âêëþ÷àÿ èíãèáèòîðû ÌÀÎ, ÒÖÀ, ÑÈÎÇÑ, ÈÎÇÑÍ – âåíëàôàêñèí (4, 27), áûëà ïðîäåìîíñòðèðîâàíà ýôôåêòèâíîñòü â ïðåäîòâðàùåíèè îáîñòðåíèé è ðåöèäèâîâ äåïðåññèè. Ñîâðåìåííûå êëèíè÷åñêèå ðóêîâîäñòâà óêàçûâàþò íà òî, ÷òî ïàöèåíòû äîëæíû ïðîäîëæàòü ëå÷åíèå â òå÷åíèå 14–20 íåäåëü ïîñëå äîñòèæåíèÿ ðåìèññèè, ñ öåëüþ ïðåäîòâðàùåíèÿ ðåöèäèâà äåïðåññèâíîãî ýïèçîäà (2). Òàêæå è ïàöèåíòû ñ âûñîêèì ðèñêîì ðàçâèòèÿ î÷åðåäíîãî äåïðåññèâíîãî ýïèçîäà äîëæíû ïðèíèìàòü ïîääåðæèâàþùóþ òåðàïèþ. Ïàöèåíòû, âêëþ÷åííûå â íàñòîÿùåå èññëåäîâàíèå, Ïðèìå÷àíèå: * – ÷àñòîòà íå ìåíåå 10% â îáåèõ òåðàïåâòè÷åñêèõ ãðóïïàõ. íåæåëàòåëüíûõ ÿâëåíèé íå áûëî ðàñöåíåíî èññëåäîâàòåëÿìè êàê ñâÿçàííîå ñ òåðàïèåé. Ñóèöèäàëüíàÿ ïîïûòêà èìåëà ìåñòî ó ïàöèåíòà èç ãðóïïû ïëàöåáî è áûëà ðàñöåíåíà èññëåäîâàòåëÿìè êàê âîçìîæíî ñâÿçàííàÿ ñ òåðàïèåé. Äàííûé ìóæ÷èíà 56 ëåò óæå èìåë â àíàìíåçå ñóèöèäàëüíóþ ïîïûòêó. Îí ïîëó÷àë öèòàëîïðàì â òå÷åíèå 56 äíåé êóïèðóþùåé ôàçû ëå÷åíèÿ, äàëåå ýñöèòàëîïðàì â ñòàáèëèçèðóþùåé ôàçå òåðàïèè â òå÷åíèå 16-òè íåäåëü, à çàòåì ïëàöåáî â ïîääåðæèâàþùåé ôàçå ëå÷åíèÿ. ×åðåç ìåñÿö ïîñëå ïðèåìà ïîñëåäíåé äîçû ïëàöåáî ïàöèåíò áûë ãîñïèòàëèçèðîâàí â ñâÿçè ñ ñóèöèäàëüíîé ïîïûòêîé, ñîâåðø¸ííîé ïóò¸ì ïåðåäîçèðîâêè ëåêàðñòâ.  ïðîìûâíûõ æèäêîñòÿõ áûë îáíàðóæåí ýñöèòàëîïðàì è àöåòàìèíîôåí. Òàê êàê ïàöèåíò ïîëó÷àë ïëàöåáî â ñëåïîì èññëåäîâàíèè, ìîæíî ïðåäïîëîæèòü, ÷òî îí íå ïîëíîñòüþ ñîáëþäàë íàçíà÷åíèÿ, ñäåëàííûå âî âðåìÿ îòêðûòîé ñòàáèëèçèðóþùåé ôàçû è íàêàïëèâàë ëåêàðñòâî. Ýñöèòàëîïðàì â ïåðèîä ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ îêàçûâàë ìèíèìàëüíîå âëèÿíèå íà ïîêàçàòåëè âèòàëüíûõ ôóíêöèé (íàïðèìåð, óðîâåíü ñèñòîëè÷åñêîãî è äèàñòîëè÷åñêîãî äàâëåíèÿ, ×ÑÑ) è íå îòëè÷àëñÿ ñóùåñòâåííî ïî ýòîìó âîçäåéñòâèþ îò ïëàöåáî (òàáë. 6). Òàêæå íå áûëî âûÿâëåíî çíà÷è- Òàáëèöà 6 Показатели жизненных функций и вес в течение двойной слепой фазы поддерживающего лечения (завершившие исследование пациенты) Èçìåðåíèå Ýñöèòàëîïðàì (n=73) Ïëàöåáî (n=66) Ñèñòîëè÷åñêîå àðòåðèàëüíîå äàâëåíèå, ìì ðò ñò p 0,509 Íà÷àëî èññëåäîâàíèÿ 119,1±14,5 118,3±15,4 -1,3±13,5 0,6±13,1 Íà÷àëî èññëåäîâàíèÿ 76,2±8,7 75,4±9,2 Çàâåðøåíèå èññëåäîâàíèÿ -0,7±8,8 1,9±8,3 Íà÷àëî èññëåäîâàíèÿ 72,3±8,4 71,3±9,6 Çàâåðøåíèå èññëåäîâàíèÿ 1,0±10,3 2,2±9,1 188,5±54,2 177,4±46,9 2,9±10,3 1,2±10,2 Çàâåðøåíèå èññëåäîâàíèÿ Äèàñòîëè÷åñêîå àðòåðèàëüíîå äàâëåíèå, ìì ðò ñò 0,133 Ïóëüñ (óä/ìèí) 0,948 Âåñ, ôóíòû 0,366 Íà÷àëî èññëåäîâàíèÿ Çàâåðøåíèå èññëåäîâàíèÿ 84 èìåëè â àíàìíåçå â ñðåäíåì îêîëî ïÿòè äåïðåññèâíûõ ýïèçîäîâ. Íàèáîëåå çíà÷èìûì ïðåäèêòîðîì âîçìîæíîãî ðàçâèòèÿ ðåöèäèâà çàáîëåâàíèÿ ÿâëÿåòñÿ êîëè÷åñòâî ïåðåíåñåííûõ ýïèçîäîâ â àíàìíåçå; ðèñê ðàçâèòèÿ ïîñëåäóþùåãî ðåöèäèâà ñîñòàâëÿåò áîëåå ÷åì 95% ó ïàöèåíòîâ ñ òðåìÿ è áîëüøèì êîëè÷åñòâîì ïðåäøåñòâóþùèõ ýïèçîäîâ (19). Ïîýòîìó ïàöèåíòàì ñ õðîíè÷åñêîé èëè ðåêóððåíòíîé äåïðåññèåé, ïåðåíåñøèì 3 èëè áîëåå äåïðåññèâíûõ ýïèçîäîâ â òå÷åíèå æèçíè, ðåêîìåíäóåòñÿ ñ ïðîôèëàêòè÷åñêîé öåëüþ ïðèåì ïîääåðæèâàþùåé òåðàïèè (40).  òî âðåìÿ êàê â ðóêîâîäñòâàõ íå ïðèâîäÿòñÿ îñîáûå ðåêîìåíäàöèè â îòíîøåíèè òèïà èëè ïðîäîëæèòåëüíîñòè ïîääåðæèâàþùåé òåðàïèè, â íèõ óêàçûâàåòñÿ íà òî, ÷òî òåðàïèÿ, êîòîðàÿ áûëà ýôôåêòèâíà â êóïèðóþùåé è ñòàáèëèçèðóþùåé ôàçå ëå÷åíèÿ äîëæíà áûòü ïðîäîëæåíà â ïîääåðæèâàþùåé ôàçå â òîé æå äîçèðîâêå ïðèìåíÿåìîãî àíòèäåïðåññàíòà. Ñîîáùàåòñÿ òàêæå è òî, ÷òî ïàöèåíòû ñî ñòàáèëüíûì ñîñòîÿíèåì, äåìîíñòðèðîâàëè õóäøèå êëèíè÷åñêèå èñõîäû â ñëó÷àå óìåíüøåíèÿ äîçèðîâêè àíòèäåïðåññàíòà íà ýòàïå ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ â ñðàâíåíèè ñ òåìè, êòî ïðîäîëæèë ëå÷åíèå äîçèðîâêîé ïðåïàðàòà ýôôåêòèâíîé â êóïèðóþùåé è ñòàáèëèçèðóþùåé ôàçå òåðàïèè (7, 34). Íàëè÷èå ðåçèäóàëüíûõ ñèìïòîìîâ, ñîõðàíÿþùèõñÿ ïîñëå ðàçðåøåíèÿ äåïðåññèâíîãî ýïèçîäà, òàêæå ÿâëÿåòñÿ âàæíûì ïðåäèêòîðîì ðåöèäèâà çàáîëåâàíèÿ (16, 21, 32).  äàííîì èññëåäîâàíèè ïåðåä òåì êàê âîéòè â 3 ñòàäèþ òåðàïèè ïàöèåíòû àêòèâíî ëå÷èëèñü íà ïðîòÿæåíèè 6 ìåñÿöåâ. Èõ ñîñòîÿíèå îöåíèâàëîñü ïî øêàëå MADRS ìåíåå ÷åì â 5 áàëëîâ, ÷òî îçíà÷àëî ïîëíóþ ðåäóêöèþ äåïðåññèâíûõ ðàññòðîéñòâ (43). Òàêèì îáðàçîì, íà îñíîâàíèè ïîëó÷åííûõ äàííûõ ìîæíî ïðåäïîëîæèòü, ÷òî îòìåíà àêòèâíîé òåðàïèè ó ïàöèåíòîâ äàæå ñ íåçíà÷èòåëüíûìè ðåçèäóàëüíûìè ñèìïòîìàìè, ìîæåò çíà÷èòåëüíî ïîâûñèòü ðèñê ðàçâèòèÿ ðåöèäèâà çàáîëåâàíèÿ. Ïîýòîìó ïàöèåíòàì ñ ðåêóððåíòíûì áîëüøèì äåïðåññèâíûì ðàññòðîéñòâîì ðåêîìåíäóåòñÿ ïîääåðæèâàþùàÿ òåðàïèÿ íà ïðîòÿæåíèè 4–6 ìåñÿöåâ ïîñëå ïîëíîãî ðàçðåøåíèÿ ñèìïòîìîâ çàáîëåâàíèÿ äàæå ïðè íåçíà÷èòåëüíîé ðåçèäóàëüíîé ñèìïòîìàòèêå (30). Òåðàïèÿ ýñöèòàëîïðàìîì õîðîøî ïåðåíîñèëàñü ïàöèåíòàìè, è âñå âîçíèêàâøèå íåæåëàòåëüíûå ÿâëåíèÿ áûëè âûðàæåíû óìåðåííî, ÷òî ñîîòâåòñòâîâàëî äàííûì äðóãèõ èññëåäîâàíèé (1, 3, 22, 28, 34). Ãîëîâîêðóæåíèå – ñèìïòîì, ïðîÿâëÿþùèéñÿ ïðè ïðåêðàùåíèè ïðè¸ìà ÑÈÎÇÑ, áûëî îòìå÷åíî ó ïàöèåíòîâ, ïîëó÷àâøèõ ïëàöåáî â ïîääåðæèâàþùóþ ôàçó ëå÷åíèÿ. Õîòÿ ýòî âñåãî ëèøü îäíî èç ïðîÿâëåíèé ñèíäðîìà îòìåíû ÑÈÎÇÑ, îíî èñïîëüçîâàëîñü äëÿ îöåíêè âûðàæåííîñòè âëèÿíèÿ ïðåêðàùåíèÿ òåðàïèè íà ðàçâèòèå íåæåëàòåëüíûõ ÿâëåíèé ó ïàöèåíòîâ, ïåðåøåäøèõ ñ ïðèåìà ýñöèòàëîïðàìà â îòêðûòîé ôàçå èññëåäîâàíèÿ íà ïëàöåáî â äâîéíîé ñëåïîé ôàçå ïîääåðæèâàþùåãî ëå÷åíèÿ.  íà÷àëå áîëåå ÷àñòûå æàëîáû íà ãîëîâîêðóæåíèå îòìå÷àëèñü â ãðóïïå, ïîëó÷àþùèõ ïëàöåáî, â ñðàâíåíèè ñ ãðóïïîé, ïðîäîëæàþùèõ ïîëó÷àòü ýñöèòàëîïðàì. Ïðè ýòîì ÷àñòîòà ðàçâèòèÿ ãîëîâîêðóæåíèÿ íà ïðîòÿæåíèè ïåðâûõ 14 äíåé ïðèìåíåíèÿ ïëàöåáî ñíèçèëàñü ñ 18% äî 2%. Áîëüøèíñòâî ïàöèåíòîâ, ñîîáùàâøèõ î ãîëîâîêðóæåíèè, êàê î íåæåëàòåëüíîì ÿâëåíèè, âîçíèêøåì â ñâÿçè ñ òåðàïèåé â ïåðâûå 14 äíåé ïîääåðæèâàþùåé ôàçû ëå÷åíèÿ, äî ýòîãî ïîëó÷àëè ýñöèòàëîïðàì â äîçèðîâêå 20 ìã/ñóò, êîòîðûé áûë îòìåíåí îäíîìîìåíòíî.  ðåàëüíîé ïðàêòèêå ïàöèåíòû áûëè áû ïåðåâåäåíû íà òåðàïèþ ýñöèòàëîïðàìîì â äîçèðîâêå 10 ìã/ñóò è äàëåå 5 ìã/ñóò ïðåæäå, ÷åì ïðåêðàòèòü òåðàïèþ ïîëíîñòüþ.  öåëîì, ïîääåðæèâàþùàÿ òåðàïèÿ ýñöèòàëîïðàìîì õîðîøî ïåðåíîñèëàñü è áûëà ýôôåêòèâíîé â ïðåäîòâðàùåíèè ðàçâèòèÿ ðåöèäèâîâ, ÷òî ïîäòâåðäèëî äàííûå ðàíåå ïðîâåä¸ííûõ èññëåäîâàíèé (4, 24, 34, 41). Òàêèì îáðàçîì, ïîëó÷åííûå äàííûå ñâèäåòåëüñòâóþò òîì, ÷òî ýñöèòàëîïðàì ÿâëÿåòñÿ ýôôåêòèâíûì àíòèäåïðåññàíòîì äëÿ ïîääåðæèâàþùåé òåðàïèè ðåêóððåíòíîãî áîëüøîãî äåïðåññèâíîãî ðàññòðîéñòâà. ËÈÒÅÐÀÒÓÐÀ recurrent depression // J. Affect. Disord. – 1993. – Vol. 27. – P. 139– 145. 9. Frank E., Kupfer D.J., Perel J.M. et al. Three-year outcomes for maintenance therapies in recurrent depression // Arch. Gen. Psychiatry. – 1990. – Vol. 47. – P. 1093–1099. 10. Geddes J.R., Carney S.M., Davies C. et al. Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review // Lancet. – 2003. – Vol. 361. – P. 653–661. 11. Gilaberte I., Montejo A.L., de la Gandara J. et al. Fluoxetine in the prevention of depressive recurrences: a double-blind study // J. Clin. Psychopharmacol. – 2001. – Vol. 21. – P. 417–424. 12. Guy W. ECDEU Assessment Manual for PsychopharmacologyRevised. US Dept Health, Education, and Welfare publication (ADM) 76338. – Rockville, Md: National Institute of Public Health, 1976. – P. 218– 222. 13. Hamilton M. A rating scale for depression // J. Neurol. Neurosurg. Psychiatry. – 1960. – Vol. 23. – P. 56–62. 14. Hirschfield R.M. Antidepressants in long-term therapy: a review of tricyclic antidepressants and selective serotonin reuptake inhibitors // Acta Psychiatr. Scand. – 2000. – Vol. 403. – P. 35–38. 15. Hochstrasser B., Isaksen P.M., Koponen H. et al. Prophylactic effect of citalopram in unipolar, recurrent depression: placebo-controlled 1. Allgulander C., Florea I., Huusom A.K. Prevention of relapse in generalized anxiety disorder by escitalopram treatment // Int. J. Neuropsychopharmacol. – 2005. – Vol. 1. – P. 11. 2. American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder (Revision) // Am. J. Psychiatry. – 2000. – Vol. 157, Suppl. 4. – P. 1–45. 3. Bielski R.J., Bose A., Chang C.C. A double-blind comparison of escitalopram and paroxetine in the long-term treatment of generalized anxiety disorder // Ann. Clin. Psychiatry. – 2005. – Vol. 17. – P. 65–69. 4. Burke W.J., Gergel I., Bose A. Fixed-dose trial of the single isomer SSRI escitalopram in depressed outpatients // J. Clin. Psychiatry. – 2002. – Vol. 63. – P. 331–336. 5. Duboff E.A. Long-term treatment of major depressive disorder with paroxetine // J. Clin. Psyñhopharmacol. – 1993. – Vol. 13. – P. 28S– 33S. 6. Forest Laboratories Clinical Trial Registry. Available at: www.forestclinicaltrials.com. Accessed March 16, 2006. 7. Franchini L., Gasperini M., Perez J. et al. Dose-response efficacy of paroxetine in preventing depressive recurrences: a randomized, doubleblind study // J. Clin. Psychiatry. – 1998. – Vol. 59. – P. 229–232. 8. Frank E., Kupfer D.J., Perel J.M. et al. Comparison of full-dose versus half-dose pharmacotherapy in the maintenance treatment of 85 30. Nierenberg A.A., Peterson T.J., Alpert J.E. Prevention of relapse and recurrence in depression: the role of long-term pharmacotherapy and psychotherapy // J. Clin. Psychiatry. – 2003. – Vol. 64, Suppl. 15. – P. 13–17. 31. NIMH/NIH Consensus Development Conference statement: mood disorders: pharmacologic prevention of recurrences // Am. J. Psychiatry. – 1985. – Vol. 142. – P. 469–476. 32. Paykel E.S., Ramana R., Cooper Z. et al. Residual symptoms after partial remission: an important outcome in depression // Psychol. Med. – 1995. – Vol. 25. – P. 1171–1180. 33. Prien R.F., Kupfer D.J., Mansky P.A. et al. Drug therapy in the prevention of recurrences in unipolar and bipolar affective disorders: report of the NIIMH collaborative study group comparing lithium carbonate, imipramine, and a lithium carbonate-imipramine combination // Arch. Gen. Psychiatry. – 1984. – Vol. 41. – P. 1096–1104. 34. Rapaport M.H., Bose A., Zheng H. Escitalopram continuation treatment prevents relapse of depressive episodes // J. Clin. Psychiatry. – 2004. – Vol. 65. – P. 44–49. 35. Reynolds C.F. 3rd, Frank E., Perel J.M. et al. Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: a randomized controlled trial in patients older than 59 years // JAMA. – 1999. – Vol. 281. – P. 39–45. 36. Rybakowski J.K., Nawacka D., Kiejna A. One-year course of the first vs multiple episodes of depression: Polish naturalistic study // Eur. Psychiatry. – 2004. – Vol. 19. – P. 258–263. 37. Schatzberg A.F., Haddad P., Kaplan E.M. et al. Serotonin reuptake inhibitor discontinuation syndrome: a hypothetical definition. Discontinuation Consensus panel // J. Clin. Psychiatry. – 1997. – Vol. 58, Suppl. 7. – P. 5–10. 38. Solomon D.A., Keller M.B., Leon A.C. et al. Multiple recurrences of major depressive disorder // Am. J. Psychiatry. – 2000. – Vol. 157. – P. 229–233. 39. Terra J.L., Montgomery S.A. Fluvoxamine prevents recurrence of depression: results of a long-term, double-blind, placebo-controlled study // Int. Clin. Psychopharmacol. – 1998. – Vol. 13. – P. 55–62. 40. Thase M.E. Long-term nature of depression // J. Clin. Psychiatry. – 1999. – Vol. 60, Suppl. 14. – P. 3–9. 41. Wade A., Michael Lemming O., Bang Hedegaard K. Escitalopram 10 mg/day is effective and well tolerated in a placebo-controlled study in depression in primary care // Int. Clin. Psychopharmacol. – 2002. – Vol. 17. – P. 95–102. 42. Zimbroff D., Bose A., Dayong L. Escitalopram treatment of nonresponders can lead to remission in patients who fail initial SSRI therapy. Presented at the 157th annual meeting of the American Psychiatric Association. – New York, 2004. 43. Zimmerman M., Chelminski I., Posternak M. A review of studies of the Montgomery-Asberg Depression Rating Scale in controls: implications for the definition of remission in treatment studies of depression // Int. Clin. Psychopharmacol. – 2004. – Vol. 19. – P. 1–7. study of maintenance therapy // Br. J. Psychiatry. – 2001. – Vol. 178. – P. 304–310. 16. Judd L.L., Akiskal H.S., Maser J.D. et al. Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse // J. Affect. Disord. – 1998. – Vol. 50. – P. 97–108. 17. Judd L.L. The clinical course of unipolar major depressive disorders // Arch. Gen. Psychiatry. – 1997. – Vol. 54. – P. 989–991. 18. Katz M.M., Secunda S.K., Hirschfeld R.M. et al. NIMH clinical research branch collaborative program on the psychobiology of depression // Arch. Gen. Psychiatry. – 1979. – Vol. 36. – P. 765–771. 19. Keller M.B., Boland R.J. Implications of failing to achieve successful long-term maintenance treatment of recurrent unipolar major depression // Biol. Psychiatry. – 1998. – Vol. 44. – P. 348–360. 20. Keller M.B., Kocsis J.H., Thase M.E. et al. Maintenance phase efficacy of sertraline for chronic depression: a randomized controlled trial // JAMA. – 1998. – Vol. 280. – P. 1665–1672. 21. Kennedy N., Paykel E.S. Residual symptoms at remission from depression: impact on long-term outcome // Affect. Disord. – 2004. – Vol. 80. – P. 135–144. 22. Lader M., Stender K., Burger V. et al. Efficacy and tolerability of escitalopram in 12- and 24-week treatment of social anxiety disorder: randomised, double-blind, placebo-controlled, fixed-dose study // Depress. Anxiety. – 2004. – Vol. 19. – P. 241–248. 23. Lepine J.P., Caillard V., Bisserbe J.C. et al. A randomized, placebocontrolled trial of sertraline for prophylactic treatment of highly recurrent major depressive disorder // Am. J. Psychiatry. – 2004. – Vol. 161. – P. 836–842. 24. Lepola U.M., Loft H., Reines E.H. Escitalopram (10–20 mg/day) is effective and well tolerated in a placebo-controlled study in depression in primary care // Int. Clin. Psychopharmacol. – 2003. – Vol. 18. – P. 211–217. 25. Montgomery S., Asberg M. A new depression scale designed to be sensitive to change // Br. J. Psychiatry. – 1979. – Vol. 134. – P. 382– 389. 26. Montgomery S.A., Dufour H., Brion S. et al. The prophylactic efficacy of fluoxetine in unipolar depression // Br. J. Psychiatry. – 1988. – Suppl. 3. – P. 69–76. 27. Montgomery S.A., Entsuah R., Hackett D. et al. Venlafaxine versus placebo in the preventive treatment of recurrent major depression // J. Clin. Psychiatry. – 2004. – Vol. 65. – P. 328–336. 28. Montgomery S.A., Nil R., Durr-Pal N. et al. A 24-week randomized, double-blind, placebo-controlled study of escitalopram for the prevention of generalized social anxiety disorder // J. Clin. Psychiatry. – 2005. – Vol. 66. – P. 1270–1278. 29. Mueller T.I., Leon A.C., Keller M.B. et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up // Am. J. Psychiatry. – 1999. – Vol. 156. – P. 1000–1006. ESCITALOPRAM MAINTENANCE TREATMENT FOR PREVENTION OF RECURRENT DEPRESSION: A RANDOMIZED, PLACEBO-CONTROLLED TRIAL S. G. Kornstein, A. Bose, D. Li, K. G. Saikali, Ch. Gandhi Background: Major depressive disorder is a recurrent illness that often requires maintenance antidepressant treatment. Escitalopram is a selective serotonin reuptake inhibitor (SSRI) that has shown efficacy in both acute and continuation treatment of major depressive disorder. The current trial examined the efficacy of maintenance escitalopram treatment in preventing depression recurrence in patients who responded to acute SSRI therapy. Method: Patients with recurrent DSM-IV-defined major depressive disorder (> 2 previous episodes; baseline Montgomery-Asberg Depression Rating Scale [MADRS] score >22) who had responded (MADRS score <12) to acute open-label treatment (8 weeks) with 1 of 4 SSRIs (fluoxetine, serlraline, paroxetine, or citalopram) received open-label, flexible-dose continuation treatment (16 weeks) with escitalopram (10– 20 mg/day). At the end of continuation treatment, patients maintaining response criteria were randomly assigned to 52 weeks of double-blind, fixed-dose maintenance treatment with escitalopram (10 or 20 mg/day) or placebo. Recurrence was defined as a MADRS score >22 or insufficient therapeutic response during the double-blind phase. The study was conducted between October 16, 2000, and February 4, 2003. Results: A total of 234 patients who responded to acute open-label treatment with 1 of 4 SSRIs received at least 1 dose of open-label escitalopram continuation treatment. Of 164 patients who completed escitalopram continuation treatment, 139 were randomly assigned to double-blind maintenance treatment with escitalopram (N=73) or placebo (N=66). Mean baseline MADRS scores at the start of the maintenance phase were <5 for both the placebo- and escitalopram-treatment groups. Time to recurrence was significantly longer in patients who received maintenance treatment with escitalopram compared with patients switched to placebo (hazard ratio =0.26, 95% CI=0.13 to 0.52, p<0.001). Longterm escitalopram treatment was well tolerated. Conclusion: Maintenance treatment with escitalopram was well tolerated and significantly reduced the risk for recurrence of depression. Patients with few residual symptoms following continuation treatment with escitalopram experienced a high rate of depression recurrence when switched to placebo, demonstrating the need for maintenance therapy of recurrent major depressive disorder beyond 4 to 6 months of initial symptom resolution even if few residual symptoms are present. 86